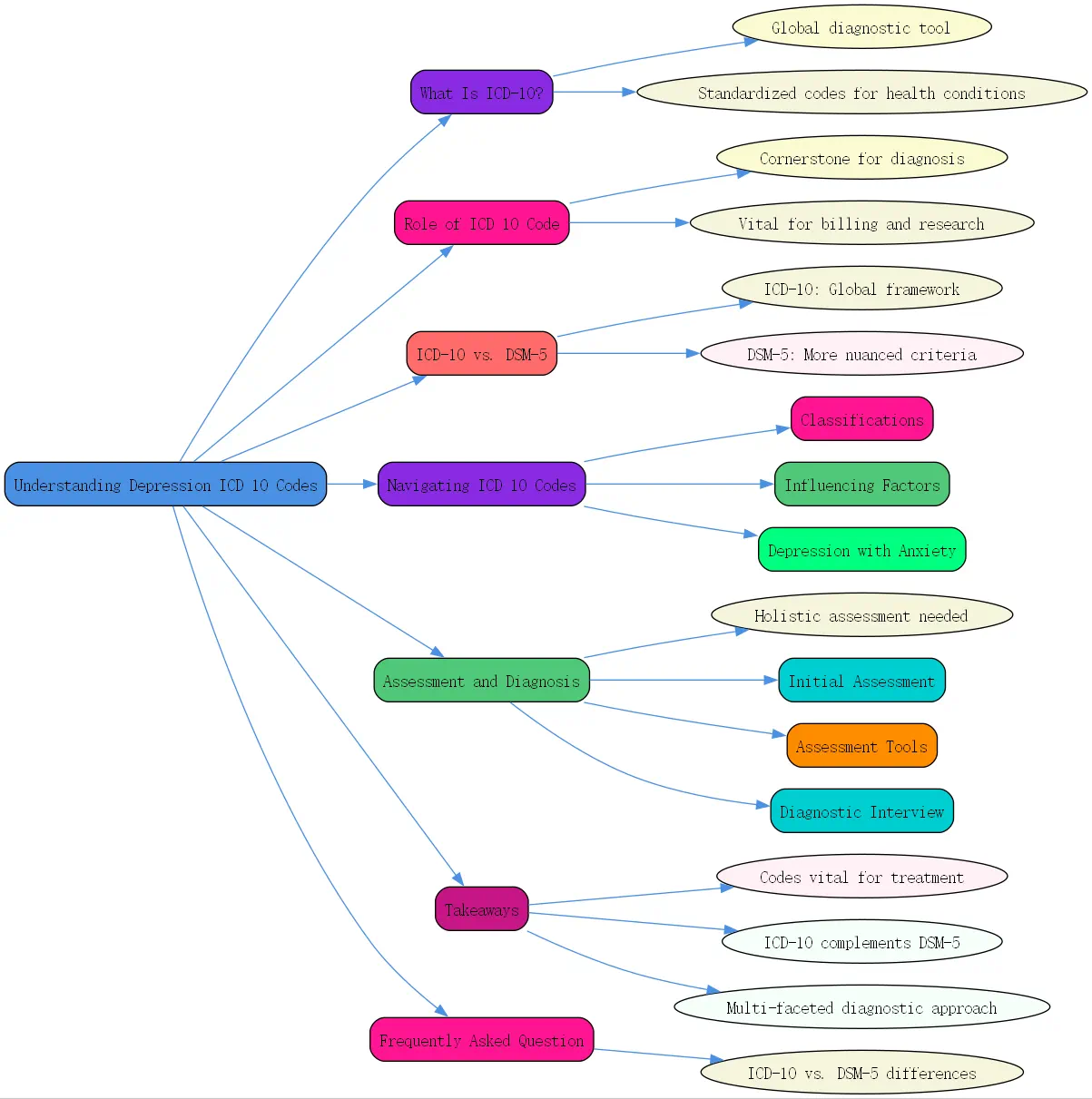
What Is ICD-10?
The International Classification of Diseases, 10th Revision (ICD-10), is a globally recognized diagnostic tool developed by the World Health Organization (WHO). It provides standardized codes used by healthcare professionals to diagnose and document physical and mental health conditions. Covering a broad spectrum of diseases, including psychological disorders, ICD-10 ensures uniformity and accuracy in healthcare communications globally.
In mental health, particularly for depression, ICD-10 is instrumental in establishing diagnostic criteria. It enables clinicians to communicate findings effectively while aligning with international health standards. This classification system is pivotal in diagnosing, tracking, and addressing the growing prevalence of mental health issues globally.
The Role of ICD 10 Code Depression in Diagnosis
ICD-10 codes for depression serve as a cornerstone for mental health diagnosis. These codes are not merely for documentation; they help clinicians accurately identify the type and severity of depression, ensuring patients receive the most appropriate care. For instance, codes like F32 for Major Depressive Disorder (single episode) or F33 for recurrent depressive episodes provide specificity, aiding treatment planning.
These codes are also vital for billing, insurance reimbursement, and research. Proper coding ensures that healthcare providers get reimbursed accurately and that researchers can analyze trends and outcomes in mental health treatment effectively. By using the correct ICD-10 depression codes, clinicians contribute to a cohesive global dataset on mental health conditions.
ICD-10 vs. DSM-5 in Diagnosing Depression
While ICD-10 provides a standardized global framework, the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition) is more commonly used in the United States for diagnosing mental disorders. Both have overlapping but distinct criteria when diagnosing depression.
The ICD-10 identifies depression based on specific symptoms and severity (mild, moderate, severe) and distinguishes between single and recurrent depressive episodes. In contrast, DSM-5 provides more nuanced criteria, including episodes of atypical depression and seasonal affective disorder. The choice between the two systems often depends on the clinician’s geographical location and the healthcare setting.
Although ICD-10 is used extensively for healthcare administrative purposes like insurance coding, DSM-5 offers a more detailed psychological perspective. Clinicians must be adept at both, as accurate classification according to ICD-10 is often required in practice, even when a DSM-5-based diagnosis is made.
Navigating the ICD 10 Depression Codes
Specific ICD 10 Code Depression Classifications
ICD-10 outlines several distinct classifications for depression, ensuring specificity in diagnosis. Key categories include:
- F32: Major Depressive Disorder, single episode.
- F33: Major Depressive Disorder, recurrent episodes.
- F34.1: Persistent Depressive Disorder (also known as dysthymia).
Each category is further divided into subcategories based on severity (mild, moderate, severe) and additional features like psychosis. These codes allow mental health professionals to tailor treatment plans based on the exact nature of the depressive disorder.
Factors Influencing the ICD 10 Code Assignment
The assignment of an ICD-10 code depends on several factors related to the patient’s condition:
- Severity of Symptoms: Whether the depression is mild, moderate, or severe. This influences treatment recommendations, from therapy to medication.
- Presence of Psychotic Features: Depression with psychotic symptoms (e.g., delusions or hallucinations) must be differentiated from non-psychotic depression. Severe depression with psychosis is coded separately, ensuring precise treatment.
- Episode Classifications: Clinicians must determine whether the depression represents a single episode (F32) or is part of a recurring pattern (F33).

These factors ensure that the diagnosis reflects the individual’s clinical presentation, reducing the chances of under- or over-diagnosis.
ICD-10 Codes for Depression with Anxiety
Depression often co-occurs with anxiety, complicating diagnosis and treatment. ICD-10 addresses this overlap with specific codes such as F41.2 for mixed anxiety and depressive disorder. By coding these conditions together, clinicians can account for the intertwined nature of anxiety and depression, ensuring a comprehensive treatment plan.
Combined diagnoses help healthcare providers address both disorders simultaneously. For instance, psychotherapy for anxiety may also significantly reduce depressive symptoms, and vice versa.
Assessment and Diagnosis of Depression: A Comprehensive Approach
Effective diagnosis of depression requires more than just ticking boxes for symptoms. The process involves holistic assessment to understand the individual’s history, behavior, and unique challenges.
Initial Assessment Components
The initial phase of diagnosis involves gathering information from various sources to paint a complete picture of the individual’s mental health. This includes:
- Input from Home and School: For children, insights from parents, teachers, and caregivers are invaluable. They provide perspectives on behavior, school performance, and social relationships.
- Strengths and Accomplishments: Recognizing what the individual does well, alongside areas of concern, gives clinicians a balanced understanding. For instance, a child excelling academically but struggling socially may require different intervention than one facing challenges in both areas.
Such multi-dimensional assessments help clinicians tailor treatment plans and ensure that no critical detail is overlooked.
Utilizing Objective and Subjective Assessment Tools
Accurate diagnosis often combines objective tools and subjective measures. Standardized objective assessments, including checklists and symptom measurement scales, allow for comparison against established norms. For example, the DSM-5 Cross-Cutting Symptom Measures help identify depression-related symptoms.
Subjective tools, while less standardized, offer valuable insights into the individual’s emotional state. Examples include projective tests like the Thematic Apperception Test (TAT) or House-Tree-Person Drawings. These subjective tools are especially useful in cases involving children, where direct conversation might not yield sufficient information.
Combining both approaches ensures comprehensive diagnostic accuracy while respecting the individual’s unique circumstances.
The Diagnostic Interview: Gathering Key Information
Interviews form the backbone of any mental health assessment. They allow clinicians to explore the nuances of the individual’s symptoms, family dynamics, and social environment.
Child assessments often involve open-ended conversations, structured play, or specific diagnostic questions. However, clinicians must also navigate potential biases during interviews, especially when input comes from multiple sources. For instance, divorced parents may present conflicting accounts, which necessitates careful evaluation of motives and accuracy.
By seeking areas of agreement and understanding possible discrepancies, clinicians can arrive at a more balanced and fair diagnosis. Maintaining an empathetic and neutral standpoint ensures trust and cooperation from all involved parties.
Takeaways
- Depression ICD 10 codes like F32 and F33 are vital for diagnostic accuracy and tailored treatment plans.
- ICD-10 complements DSM-5, and understanding both systems enhances diagnostic efficiency.
- Diagnosing depression requires a multi-faceted approach, combining input from various sources, objective tools, and subjective assessments.
- Accurate coding improves billing, research insights, and ultimately patient care.
Frequently Asked Question
Q: What is the difference between ICD-10 and DSM-5 when diagnosing depression?
A: ICD-10 and DSM-5 provide overlapping yet distinct criteria for diagnosing depression. ICD-10 emphasizes the classification of diseases globally, focusing on coding for administrative and clinical utility. For depression, ICD-10 codes like F32 (single episode) and F33 (recurrent episodes) offer practical categorization.
On the other hand, DSM-5 offers more detailed diagnostic criteria, including specific nuances like atypical depression or seasonal patterns. While clinicians worldwide often rely on ICD-10 for documentation, DSM-5 offers deeper insights into psychological mechanisms behind depression. Using both systems enhances diagnostic precision and treatment outcomes.

By integrating tools like ICD-10 and DSM-5 into comprehensive assessments, clinicians address both the biological and psychological aspects of mental health conditions, benefiting patients and public health systems alike.





