Understanding Severe Depression
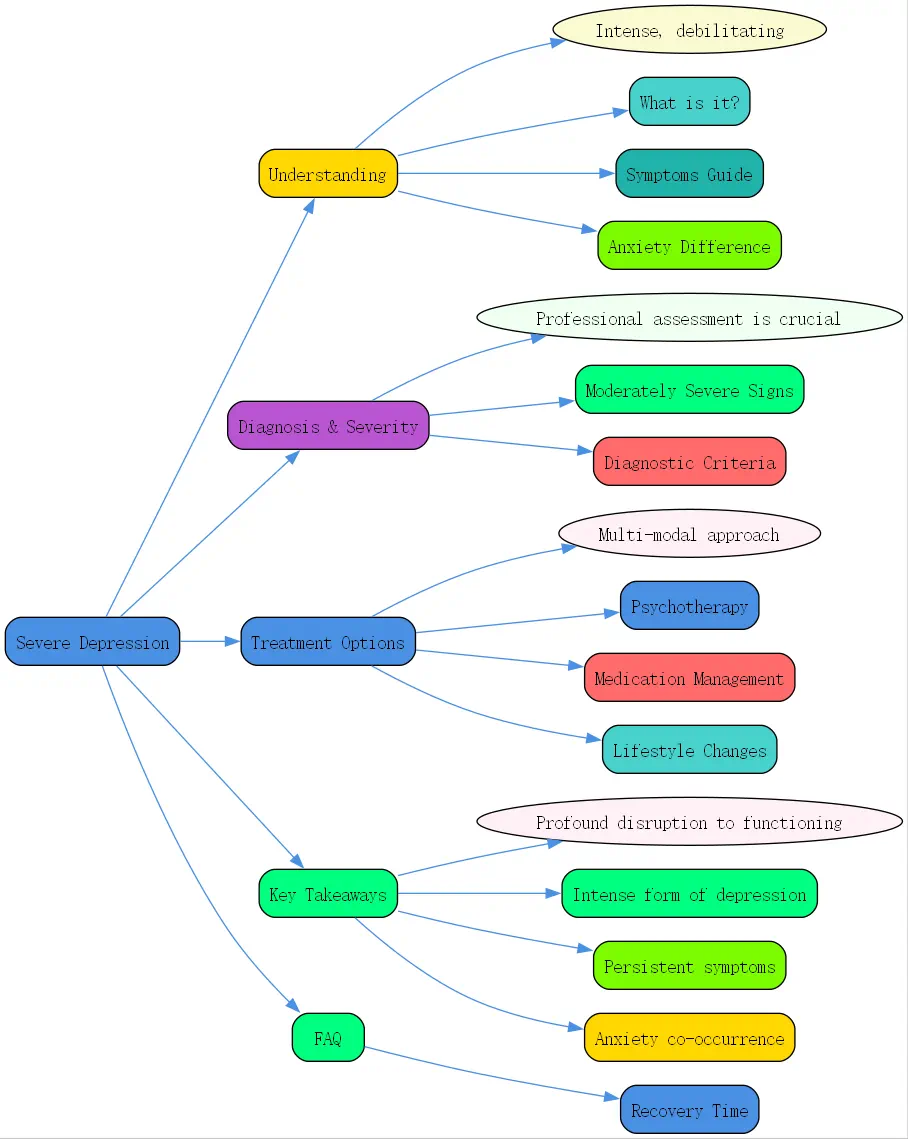
Depression exists on a spectrum of severity, with severe depression representing the most intense and debilitating form of this condition. In this comprehensive guide from BrainTalking, we’ll explore what severe depression entails, how to recognize its symptoms, and the most effective treatment approaches available today.
What is Severe Depression?
Severe depression, also known as major depressive disorder with severe features, represents the most intense form of clinical depression. Unlike milder forms of depression that might allow individuals to maintain some daily functioning, severe depression can be completely debilitating, making even basic self-care tasks seem insurmountable.
Severe depression is characterized by persistent and intense negative emotions, significant changes in physical functioning, and profound disruptions to one’s ability to work, maintain relationships, or engage in previously enjoyable activities. The condition affects both mind and body, creating a comprehensive state of suffering that requires professional intervention.
Unlike temporary feelings of sadness that everyone experiences, severe depression isn’t something a person can simply “”snap out of”” or overcome through willpower alone. It represents a serious mental health condition requiring clinical attention and comprehensive treatment.
Severe Depression Symptoms: A Comprehensive Guide

Identifying severe depression requires recognizing a constellation of symptoms that persist for at least two weeks and represent a change from previous functioning. These symptoms span emotional, cognitive, and physical domains.
Emotional and Psychological Symptoms
The emotional landscape of severe depression is bleak and overwhelming. Individuals often experience:
- Persistent feelings of sadness, emptiness, or hopelessness
- Pronounced irritability or frustration, even over minor matters
- Loss of interest or pleasure in nearly all activities (anhedonia)
- Feelings of worthlessness or excessive, inappropriate guilt
- Recurrent thoughts of death or suicide
- Difficulty concentrating, thinking clearly, or making decisions
- Slowed thinking, speaking, or body movements (psychomotor retardation)
These emotional symptoms often feel unrelenting, with little or no relief throughout the day. Unlike normal emotional responses to difficult life events, these feelings don’t improve with positive circumstances or supportive environments.
Physical Symptoms Associated with Severe Depression
Severe depression manifests physically in numerous ways, highlighting how this condition affects the entire body:
- Significant changes in appetite and weight (either increase or decrease)
- Severe sleep disturbances (insomnia or hypersomnia)
- Fatigue or loss of energy nearly every day
- Unexplained physical problems like headaches or back pain
- Digestive issues that don’t respond to treatment
These physical symptoms often compound the emotional distress, creating a cycle where physical discomfort worsens psychological symptoms and vice versa.

The Impact on Daily Life and Functioning
Perhaps the most distinctive feature of severe depression is its profound impact on daily functioning:
- Inability to perform at work or school
- Withdrawal from social activities and relationships
- Neglect of personal hygiene and self-care
- Difficulty completing even basic tasks like showering or preparing meals
- Complete loss of motivation for previously valued activities
This level of impairment distinguishes severe depression from milder forms and underscores the urgent need for comprehensive treatment.
Differentiating Severe Depression from Anxiety
While depression and anxiety are distinct conditions, they frequently co-occur, creating complex clinical presentations that require nuanced understanding.
The Interplay Between Anxiety and Severe Depression
Anxiety and severe depression often interact in complex ways. While depression typically involves feelings of hopelessness, worthlessness, and a lack of energy, anxiety centers on excessive worry, fear, and physiological arousal.
The relationship between these conditions is bidirectional—anxiety can trigger depressive episodes, while depression can intensify anxious thoughts. Understanding this interplay is crucial for accurate diagnosis and effective treatment.
Anxiety Severe Depression: Understanding Comorbidity
The co-occurrence of anxiety and severe depression, known as comorbidity, is extremely common. Research suggests that approximately 60% of individuals with major depression also meet criteria for an anxiety disorder. This combination often results in:
- More severe symptoms overall
- Greater functional impairment
- Increased suicide risk
- Longer duration of illness
- Poorer response to treatment
- Higher rates of substance use
When these conditions co-exist, treatment approaches must address both simultaneously rather than focusing on one to the exclusion of the other.
Recognizing Symptoms of Both Conditions
Identifying when both anxiety and severe depression are present requires recognizing their distinctive symptom patterns:
Anxiety symptoms often include:
- Excessive worry about multiple areas of life
- Restlessness or feeling “”on edge””
- Muscle tension
- Sleep disturbances (particularly difficulty falling asleep)
- Difficulty concentrating due to worry
When combined with the core symptoms of severe depression mentioned earlier, these anxiety features create a particularly distressing experience that requires specialized treatment approaches.
Diagnosis and Severity of Depression
Professional assessment plays a crucial role in accurately diagnosing and determining the severity of depression.
Moderately Severe Depression: Identifying the Signs
Moderately severe depression occupies the middle ground between mild and severe depression. Understanding this level of severity helps in proper assessment and treatment planning.
Characteristics of Moderately Severe Depression
Moderately severe depression shares many symptoms with severe depression but may differ in intensity or functional impact:
- Symptoms are clearly noticeable and disruptive but may not completely prevent functioning
- Individuals may still maintain some work or social activities, though with significant difficulty
- Self-care may be diminished but not entirely neglected
- Suicidal thoughts may be present but without specific plans
- Some response to positive events may still occur, though diminished
Moderately severe depression represents a serious condition requiring prompt attention, as it can readily progress to severe depression without appropriate intervention.
When to Seek Professional Help
Recognizing when to seek help for moderately severe depression is crucial. Consider reaching out to a mental health professional if:
- Symptoms persist for more than two weeks
- Functioning at work, school, or in relationships is significantly impaired
- Self-care has diminished noticeably
- Sleep or appetite has changed dramatically
- Thoughts of death or suicide are present, even if passive
- Attempts to manage symptoms on your own haven’t been successful
Early intervention for moderately severe depression can prevent progression to more severe states and improve treatment outcomes.
Diagnostic Criteria for Severe Depression
Formal diagnosis of severe depression follows established clinical guidelines that ensure consistency in assessment and treatment planning.
DSM-5 Criteria for Major Depressive Disorder (Severe)
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), major depressive disorder with severe features requires:
1. Five or more symptoms present during the same 2-week period, representing a change from previous functioning 2. At least one symptom must be either depressed mood or loss of interest/pleasure 3. The severity specifier “”with severe features”” indicates that almost all core symptoms are present, and the symptoms markedly interfere with social and occupational functioning 4. Symptoms cause clinically significant distress or impairment 5. Symptoms are not attributable to another medical condition or substance
This structured approach ensures that severe depression is accurately distinguished from other conditions with overlapping symptoms.
The Role of Professional Assessment
Professional assessment for severe depression typically involves:
- Clinical interviews to gather detailed symptom history
- Standardized rating scales (like the PHQ-9 or Hamilton Depression Rating Scale)
- Medical evaluations to rule out physical causes
- Assessment of suicide risk
- Evaluation for co-occurring conditions
This comprehensive assessment approach enables clinicians to develop targeted treatment plans that address the specific features of each individual’s experience with severe depression.
Treatment Options for Severe Depression
Effective treatment for severe depression typically involves a multi-modal approach combining psychotherapy, medication, and lifestyle modifications.
Psychotherapy for Severe Depression
Psychotherapy represents a cornerstone of treatment for severe depression, offering evidence-based approaches to addressing underlying thought patterns and behaviors.
Cognitive Behavioral Therapy (CBT) and its Effectiveness
Cognitive Behavioral Therapy has demonstrated robust effectiveness for severe depression. This structured approach:
- Identifies and challenges negative thought patterns
- Develops behavioral activation strategies to counter withdrawal and inactivity
- Builds problem-solving skills for managing life stressors
- Creates relapse prevention plans for long-term wellness
Research consistently shows that CBT produces significant improvements in depressive symptoms, with effects that often endure after treatment ends. At BrainTalking, we recognize CBT as a first-line treatment for severe depression based on its strong evidence base.
Other Therapeutic Approaches
While CBT is well-studied, several other therapeutic modalities show promise for severe depression:
- Interpersonal Therapy (IPT): Focuses on improving interpersonal relationships and social functioning
- Psychodynamic Therapy: Explores how unconscious processes contribute to current feelings and behaviors
- Acceptance and Commitment Therapy (ACT): Emphasizes acceptance of difficult emotions while committing to value-based actions
- Mindfulness-Based Cognitive Therapy (MBCT): Combines mindfulness practices with cognitive techniques to prevent relapse

These approaches might be particularly helpful for individuals who haven’t responded adequately to CBT or who have specific interpersonal or existential concerns underlying their depression.
Medication Management for Severe Depression
Pharmacological interventions play a crucial role in treating severe depression, particularly when symptoms significantly impair functioning.
Antidepressants: SSRIs and Other Options
Several medication classes are used to treat severe depression:
- Selective Serotonin Reuptake Inhibitors (SSRIs): Often prescribed as first-line medications due to their relative safety and tolerability
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): May be more effective for some individuals, particularly those with pain symptoms
- Atypical antidepressants: Include medications like bupropion, mirtazapine, and vortioxetine, which work through different mechanisms
- Tricyclic antidepressants and MAOIs: Older classes that may be used when other options haven’t been effective
For severe depression, medication is often considered essential, at least in the acute phase of treatment, due to the profound impairment associated with this condition.
Managing Side Effects and Finding the Right Medication
Finding the right medication often involves trial and error. Key considerations include:
- Side effects vary substantially between individuals and medications
- Full therapeutic effects typically take 4-6 weeks to emerge
- Dosage adjustments are often necessary to balance efficacy and tolerability
- Augmentation strategies (adding a second medication) may be needed for partial response
- Regular monitoring by a healthcare provider is essential
The journey to finding effective medication often requires patience and close collaboration with healthcare providers.
Lifestyle Changes and Self-Care Strategies
While professional treatments are essential for severe depression, lifestyle modifications provide important complementary support.
The Importance of Diet, Exercise, and Sleep
Research increasingly highlights how physical health practices impact depression recovery:
- Regular physical activity (even gentle movement) can significantly reduce depressive symptoms
- Nutritional approaches emphasizing whole foods, omega-3 fatty acids, and reduced processed foods may support mood regulation
- Sleep hygiene practices are essential, as both insomnia and hypersomnia can worsen depression
- Limiting alcohol and avoiding recreational drugs prevents interference with recovery
These lifestyle factors work synergistically with formal treatments to create comprehensive recovery support.
Building a Support System
Social connection plays a crucial role in depression recovery:
- Maintaining or rebuilding relationships provides emotional support and counters isolation
- Support groups connect individuals with others who understand the experience
- Family involvement in treatment enhances understanding and practical support
- Setting appropriate boundaries protects energy during the recovery process
Cultivating these supportive relationships creates a foundation for sustainable recovery from severe depression.
Key Takeaways
- Severe depression represents the most intense form of clinical depression, causing profound disruption to daily functioning
- Severe depression symptoms include emotional, cognitive, and physical manifestations that persist for at least two weeks
- Anxiety and severe depression frequently co-occur, creating complex clinical presentations requiring specialized treatment
- Moderately severe depression should be taken seriously as it can progress to severe depression without appropriate intervention
- Evidence-based treatments include psychotherapy (particularly CBT), medication, and lifestyle modifications
- Recovery typically requires a multi-modal approach combining professional help with self-care practices
- Early intervention improves outcomes and reduces suffering
Frequently Asked Questions
How long does it take to recover from severe depression?
Recovery from severe depression varies significantly between individuals. With appropriate treatment, many people begin to notice improvement within 4-6 weeks. However, complete recovery often takes several months, and some individuals may require longer-term support.
The recovery journey typically isn’t linear—improvement often comes with ups and downs. What’s most important is maintaining treatment consistency even as symptoms begin to improve. Premature discontinuation of treatment is associated with higher relapse rates. A good rule of thumb is to continue treatment for at least 6-12 months after reaching remission to consolidate gains and prevent relapse.