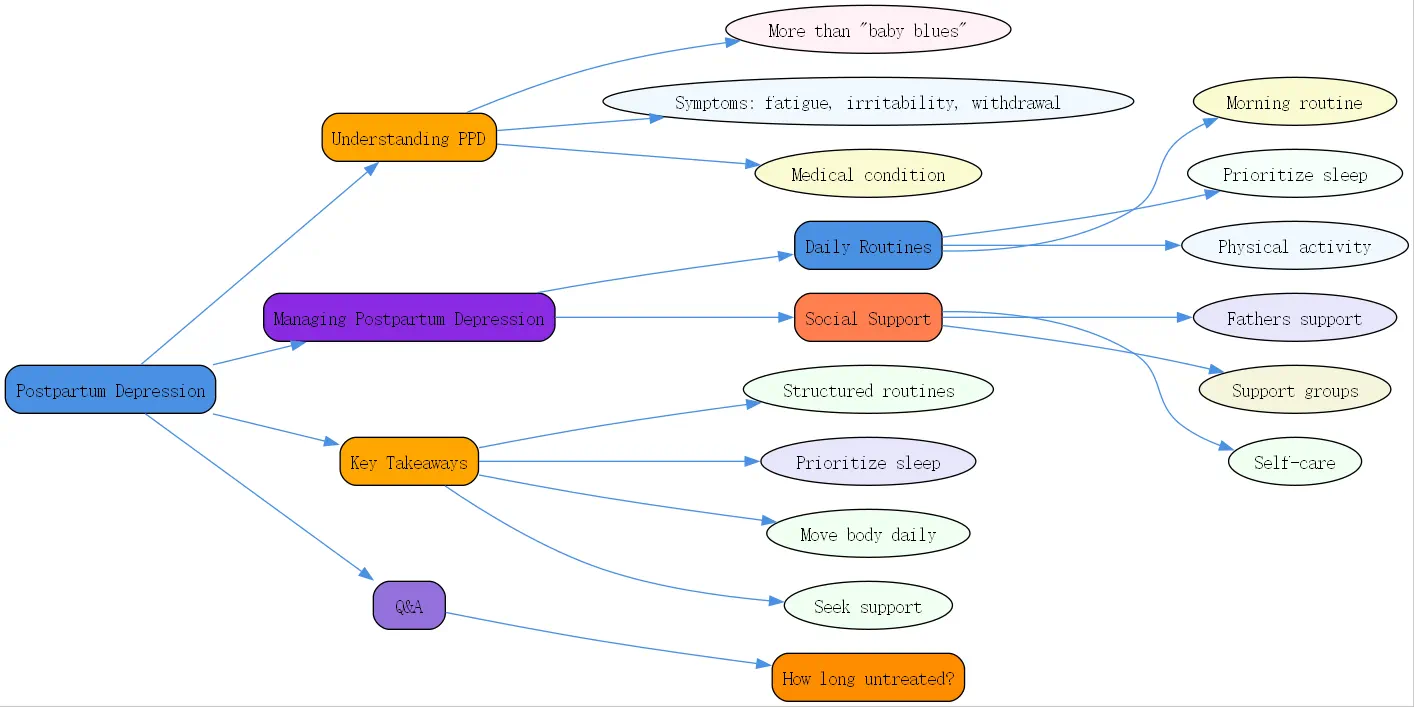
Understanding Postpartum Depression
Postpartum depression (PPD) represents more than just the “”baby blues”” that many new parents experience. It’s a serious mental health condition that affects approximately 1 in 8 women after childbirth, according to the CDC’s postpartum depression statistics. Unlike the temporary mood swings and mild anxiety that characterize baby blues, postpartum depression involves persistent feelings of sadness, emptiness, and hopelessness that can interfere with daily functioning and the ability to care for oneself and one’s baby.
The symptoms of postpartum depression often include overwhelming fatigue, intense irritability, difficulty bonding with the baby, withdrawal from family and friends, and in some cases, thoughts of harming oneself or the baby. These symptoms typically emerge within the first few weeks after delivery but can appear anytime during the first year.
At BrainTalking, we emphasize that postpartum depression is not a character flaw or a sign of weakness. Rather, it’s a medical condition influenced by physical, emotional, and hormonal changes that accompany childbirth. Understanding this distinction is crucial for seeking appropriate help and implementing effective management strategies.
Daily Routines and Strategies for Managing Postpartum and Depression
The Importance of a Morning Routine for Mental Health
Establishing a consistent morning routine can provide structure and stability during the often chaotic postpartum period. Licensed therapist Emma McAdam emphasizes beginning the day with intention rather than immediately reaching for your phone or scrolling through social media, which can trigger stress and anxiety.
Starting your day with mindfulness practices such as meditation or prayer can help center your thoughts and set a positive tone. McAdam shares, “”I express gratitude for the day and for my life and the opportunity I have to do good in the world,”” noting how this connection helps her “”feel loved and purposeful through my day.””
For those experiencing postpartum depression, setting small, achievable goals each morning can provide a sense of direction and accomplishment. This might include simple tasks like taking a shower, eating breakfast, or spending a few minutes in quiet reflection. The key is to start with manageable steps rather than overwhelming yourself with expectations.
Sleep and Postpartum Depression: Prioritizing Rest
Sleep deprivation and postpartum depression form a vicious cycle—lack of sleep can worsen depression symptoms, while depression can make it difficult to sleep even when the opportunity arises. Research indicates that 87% of people who resolved their insomnia significantly decreased their depression symptoms.
While the advice to “”sleep when the baby sleeps”” is common, implementing a consistent sleep schedule can be more beneficial. This might mean coordinating with your partner or support person to ensure you get uninterrupted rest periods. McAdam notes the importance of listening to your body’s natural biorhythms rather than fighting against them.
For those struggling with postpartum depression, prioritizing sleep might mean temporarily adjusting expectations around household chores or limiting visitors. Remember that adequate rest is not a luxury but a necessity for mental health recovery, particularly during the postpartum period.
The Power of Physical Activity and Nutrition
Exercise has been consistently shown to reduce symptoms of depression by releasing endorphins and reducing stress hormones. For new parents experiencing postpartum depression, even brief periods of physical activity can make a significant difference in mood and energy levels.
McAdam shares, “”When I exercise it just works through a backlog of pent-up emotions and I can feel my body relax. I think it also helps me deal with anger and frustration.”” The type of exercise doesn’t need to be intense—walking with the baby in a stroller, gentle postpartum yoga, or even dancing around the living room can be effective.
Nutrition also plays a crucial role in managing postpartum depression. Consuming a diet rich in omega-3 fatty acids, whole grains, lean proteins, and plenty of fruits and vegetables can support brain health and mood regulation. Limiting sugar and processed foods may help prevent energy crashes that can exacerbate feelings of fatigue and depression.
The Benefits of Spending Time in Nature
Nature exposure has been linked to reduced stress levels and improved mood, making it a valuable tool for managing postpartum depression. McAdam emphasizes, “”I need nature. I need to see the sky and soak in some sun,”” noting that research shows “”sunshine and nature and being outside changes our physiology. It slows our heart rate and decreases stress chemicals.””
For new parents who may find it challenging to get outdoors with an infant, even small doses of nature can be beneficial. This might include sitting near a window with natural light, spending time on a balcony or porch, or taking short walks in a nearby park. If getting outside isn’t possible, looking at nature photography or watching nature documentaries can provide some of the same psychological benefits.
Evening Routines for Relaxation and Reflection
Developing a calming evening routine can help signal to your body that it’s time to wind down, potentially improving sleep quality and reducing anxiety. McAdam describes taking “”quiet time for myself”” in the evening, often including a hot bath and reading.
Journaling can be particularly beneficial for those experiencing postpartum depression. McAdam shares, “”I often take the time to write about my wins and accomplishments of the day so that I can remember them because it’s my natural habit to dwell on my mistakes and shortcomings.”” This practice of acknowledging daily successes, no matter how small, can help counter the negative thought patterns common in depression.
Limiting screen time before bed is also important, as blue light can interfere with melatonin production and disrupt sleep. If you do use screens in the evening, opt for calming content rather than stimulating or potentially triggering material.
The Role of Fathers and Social Support in Postpartum Depression
Father Postpartum Depression: Recognizing Signs and Seeking Help
While postpartum depression is often associated with mothers, father postpartum depression is increasingly recognized as a significant concern. Approximately 8-10% of new fathers experience depression in the first year after their child’s birth, with symptoms that may include irritability, withdrawal, working excessively, or engaging in risky behaviors rather than the sadness typically associated with depression.
Risk factors for father postpartum depression include a partner with depression, sleep deprivation, financial stress, and a history of mental health challenges. At BrainTalking, we emphasize the importance of fathers seeking help through therapy, support groups, or medical intervention when experiencing these symptoms.

The Importance of Social Connection and Support Groups
Social isolation can significantly worsen postpartum depression, yet many new parents find themselves cut off from their usual social networks. McAdam notes, “”Having social interactions is really essential for mental health. Our brains are inherently social. We are social creatures.””

Support groups specifically for postpartum depression can provide validation, practical advice, and a sense of community. These might be in-person or online, with the latter offering flexibility for parents with unpredictable schedules. Even virtual connections through video calls with friends and family can help combat feelings of isolation.
Healthcare providers, including those at BrainTalking, can often recommend local resources for postpartum support. Partners, family members, and friends can also play crucial roles by offering practical help with baby care and household tasks, providing emotional support without judgment, and encouraging professional help when needed.
Self-Care Activities for New Parents
Self-care during the postpartum period isn’t selfish—it’s necessary for maintaining the energy and emotional resources needed to care for a newborn. McAdam shares how she schedules “”about two hours a week to do at least one of”” her hobbies, noting, “”I put it on the calendar so that I make sure it happens.””
For parents experiencing postpartum depression, self-care might initially focus on basic needs like showering, eating regular meals, and stepping outside for fresh air. As recovery progresses, incorporating activities that brought joy before parenthood—even in modified form—can help reconnect with one’s identity beyond being a parent.
Setting boundaries around visitors, social media use, and obligations can also be an important form of self-care during this vulnerable time. Learning to say no to non-essential commitments preserves energy for healing and bonding with the baby.

Managing Postpartum Depression: Key Takeaways
- Establish structured routines: Create simple morning and evening routines that provide stability and incorporate self-care.
- Prioritize sleep: Work with partners or support people to ensure you get adequate rest, even if it means adjusting other expectations.
- Move your body daily: Even gentle exercise can significantly improve mood and reduce stress hormones.
- Connect with nature: Spend time outdoors when possible, or bring elements of nature indoors.
- Seek social support: Join postpartum support groups, maintain connections with friends and family, and be honest about your struggles.
- Watch for signs in fathers: Be aware that postpartum depression affects fathers too, often with different symptoms than mothers experience.
- Practice gratitude: Acknowledge daily wins and moments of joy, no matter how small they seem.
- Get professional help: Therapy, medication, or a combination may be necessary for recovery from postpartum depression.
Q&A: Common Questions About Postpartum Depression
How long does postpartum depression typically last if left untreated?
Without treatment, postpartum depression can persist for months or even years. The duration varies widely depending on individual circumstances, severity, and environmental factors. Some parents may experience gradual improvement as hormones stabilize and they adjust to parenthood, but many continue to struggle with symptoms that can worsen over time.
Professional treatment—which may include therapy, medication, support groups, or a combination—typically accelerates recovery significantly. With appropriate intervention, many people begin to see improvement within a few weeks, though full recovery may take several months. Early intervention is key to preventing prolonged suffering and minimizing the impact on parent-child bonding and family dynamics.




