Understanding Treatment Resistant Depression
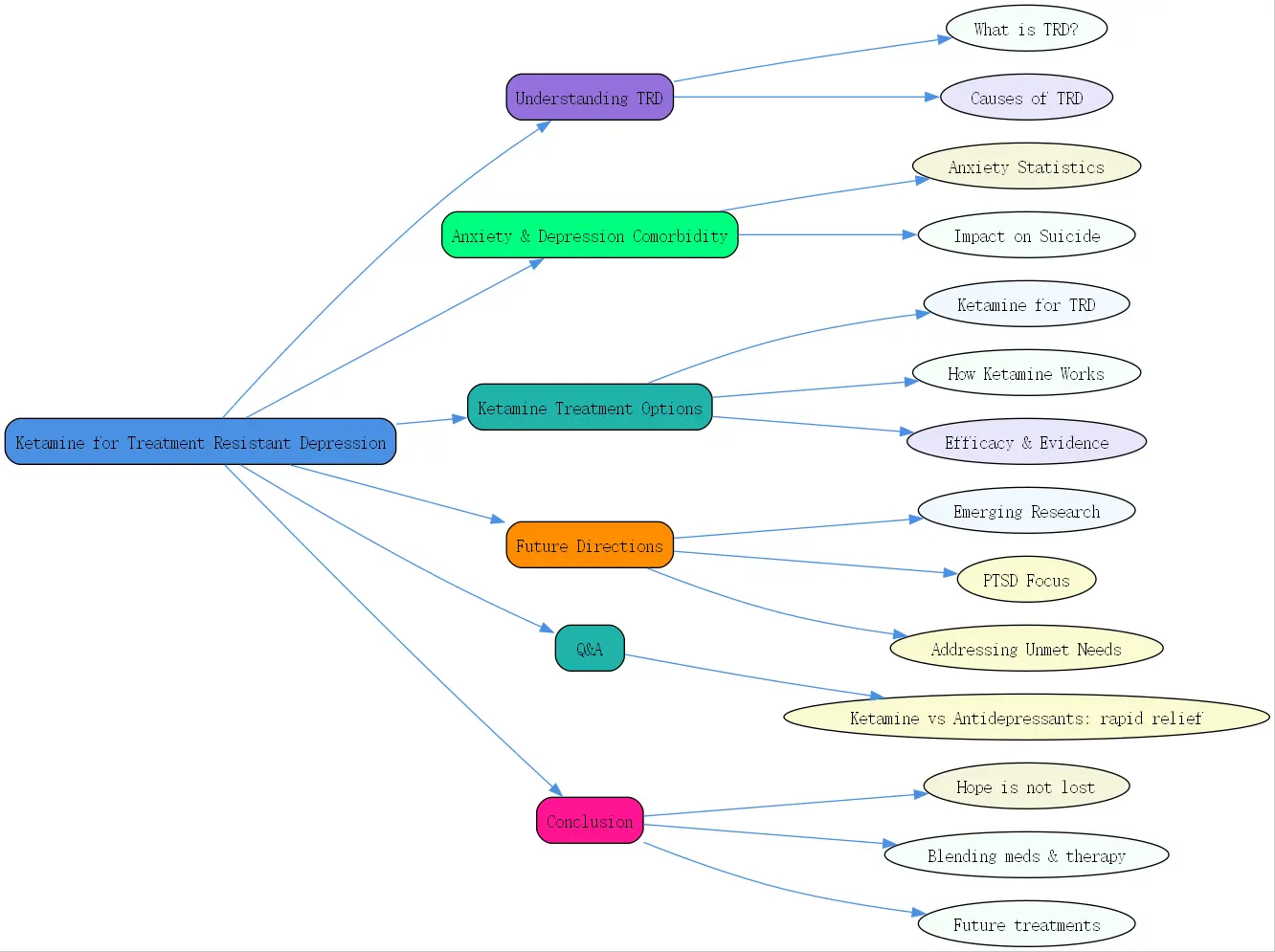
What is Treatment Resistant Depression (TRD)?
Treatment-resistant depression (TRD) is a tough reality for many. It’s defined as depression that doesn’t improve after trying at least two different antidepressants from separate classes at adequate doses and durations. Think of it as depression that’s dug in its heels, refusing to budge despite standard efforts. At BrainTalking, we recognize how frustrating this can be for patients and clinicians alike. Diagnosing TRD involves ruling out other factors like medication non-compliance or misdiagnosis, ensuring the label fits.
The condition affects a significant chunk of people with depression—about 30% don’t respond to typical treatments. That’s millions grappling with persistent sadness, fatigue, and despair. It’s not just a mood issue; it’s a life-altering challenge that demands innovative solutions.
Why Treatment Resistance Occurs
So, why does TRD happen? It’s complicated. Genetics play a big role—some folks’ brains are wired to resist certain medications due to how they process chemicals like serotonin or dopamine. Then there’s the overlap with other conditions. Anxiety disorders, substance use, or even chronic stress can throw a wrench into treatment plans, making depression harder to crack.
Environmental factors matter too. Trauma, ongoing stress, or lack of social support can deepen depression’s roots. It’s like trying to grow a plant in rocky soil—standard care might not be enough. Understanding these layers helps explain why TRD is such a stubborn foe.
The Impact of TRD on Patients’ Lives
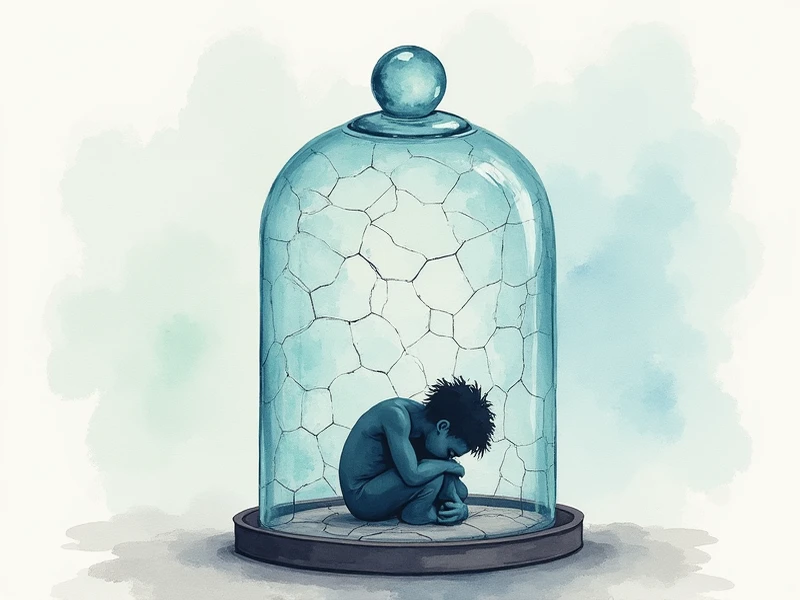
Living with TRD is exhausting. Imagine feeling hopeless day after day, with no relief in sight. It chips away at everything—work, relationships, even simple joys like a morning coffee. Patients often face higher healthcare costs, bouncing between doctors and therapies. Worse, the risk of suicide spikes as despair festers.
The disability factor is huge. TRD often hits in young adulthood, derailing careers and dreams when people should be thriving. It’s a heavy burden, both emotionally and practically, making effective treatment a lifeline worth chasing.
Prevalence and Burden of Anxiety Disorders and Comorbidity with Depression
Statistics on Anxiety Disorders (GAD, Social Anxiety, PTSD)
Anxiety disorders are everywhere. One in four adults will face one in their lifetime, according to experts like Dr. Sanjay Matthew from Baylor College of Medicine. Generalized Anxiety Disorder (GAD) affects 6.8 million U.S. adults, while social anxiety disorder touches 15 million. Post-Traumatic Stress Disorder (PTSD) isn’t far behind, impacting 7.7 million. These numbers aren’t just stats—they’re people struggling daily.
These conditions often start young, in teens or early 20s, which amplifies their toll. Unlike late-life issues like dementia, anxiety strikes during prime years, reshaping lives far too early.
Comorbidity of Anxiety Disorders with Depression
Here’s where it gets tricky: anxiety and depression love to team up. Over half of GAD patients will experience depression in their lifetime, a comorbidity that’s alarmingly common. Social anxiety and PTSD often tag along too, creating a messy mix of symptoms—worry, fear, and sadness all at once.
This overlap isn’t just inconvenient; it complicates treatment. Symptoms feed off each other, making it harder to find relief. For those with TRD, this duo can feel like an unbreakable cycle, pushing the need for targeted solutions.
Impact on Disability and Suicide Rates
The stakes are high. Anxiety and depression together are top causes of disability worldwide, especially because they hit young adults. Jobs suffer, education stalls, and social ties fray. Add TRD to the mix, and the weight becomes crushing.
Suicide rates tell a grim story. The past 15 years have seen a steady climb, with post-COVID data raising fresh alarms. Veterans and active military personnel are hit hard, but it’s a broader epidemic. When treatments fail, hope fades fast, underscoring why options like ketamine for treatment-resistant depression matter so much.
Exploring Treatment Options for Resistant Depression
Ketamine Treatment Resistant Depression
Enter ketamine—a game-changer for TRD. Once just an anesthetic, it’s now a beacon of hope for those stuck in depression’s grip. Ketamine treatment for resistant depression offers something traditional antidepressants often can’t: speed. Patients who’ve tried everything else are finding relief, and that’s no small thing.
At BrainTalking, we’ve seen the buzz around this treatment grow. It’s not a cure-all, but for many, it’s a breakthrough worth exploring with a doctor’s guidance.
How Ketamine Works for TRD
Ketamine’s magic lies in its approach. Unlike SSRIs that tweak serotonin, ketamine targets the brain’s glutamate system, specifically NMDA receptors. This shift can lift depressive symptoms in hours or days—not weeks. It’s like flipping a switch when other methods barely flicker.
This rapid action is a lifeline for those in crisis. It doesn’t replace therapy or lifestyle changes, but it buys time to build a broader plan. The science is still unfolding, but the results speak loud and clear.
Efficacy and Clinical Evidence
Does it work? Studies say yes. A 2025 meta-analysis in the American Journal of Psychiatry found ketamine significantly outpaced placebo in slashing depression symptoms. Some patients see improvement after one dose, a stark contrast to the slow grind of traditional meds.
It’s not perfect—effects can fade, requiring repeat sessions. But for treatment-resistant depression, where options are slim, ketamine’s efficacy is a ray of light backed by solid clinical evidence.
Administration and Monitoring of Ketamine
Ketamine isn’t a pill you pop at home. It’s usually given via IV in a clinic, with staff watching for side effects like dissociation or blood pressure spikes. A newer option, esketamine, comes as a nasal spray, FDA-approved for TRD since 2019. It’s more convenient but still needs oversight.
Monitoring is key. Patients might feel woozy or detached during treatment, so professionals ensure safety. It’s a controlled process, but one that’s opening doors for many.
Alternative Medications and Therapies
Ketamine’s not the only player. For TRD with anxiety or insomnia, there’s a toolbox of options:
- Non-Benzodiazepine Options for Anxiety and Insomnia: Drugs like zolpidem (Ambien) or eszopiclone (Lunesta) tackle sleep without the risks of benzos.
- Sedating Antidepressants: Trazodone, mirtazapine, and doxepin pull double duty, easing depression and helping you rest.
- Melatonin Agonists: Remelteon syncs your sleep cycle via melatonin receptors.
- Orexin Receptor Antagonists: Suvorexant and lemborexant block wakefulness signals, offering fresh insomnia relief.
These alternatives give patients and doctors flexibility, especially when ketamine isn’t the fit.
Future Directions in Treatment for Resistant Depression
Emerging Research and Clinical Trials
The future’s bright for TRD. Research in 2025 is buzzing with trials on GABAergic drugs—think benzodiazepine cousins with fewer downsides. These target GABA, the brain’s chill-out chemical, aiming for fast relief without addiction risks.
Scientists are also digging into personalized treatments. What works for one brain might flop for another, so tailoring therapies is the next frontier. It’s an exciting time for breakthroughs.
Focus on Specific Anxiety Disorders (GAD, Social Anxiety, PTSD)
Not all anxiety is the same. GAD’s constant worry, social anxiety’s dread of judgment, and PTSD’s trauma echoes need specific fixes. Drug development is zeroing in here—think meds that boost fear extinction for PTSD or calm GAD’s restless mind.
This focus could untangle the TRD-anxiety knot, offering hope where one-size-fits-all falls short.
Addressing Unmet Needs in Drug Therapy
Too many still slip through the cracks. Current drugs—SSRIs, SNRIs—help some, but side effects like weight gain or slow results frustrate others. Trials often skip the sickest patients, leaving gaps in knowledge about suicide prevention.
Future therapies aim to fill these holes with faster, safer options. It’s about meeting patients where they are, not forcing a fit.
Benzodiazepines and the Future of GABA Modulation
Benzos like Valium or Xanax are old-school anxiety busters, but they’re tricky. Dependence, tolerance, and deadly opioid combos have sparked FDA warnings in 2025. Still, prescribing’s up—doctors lean on them when other treatments lag.
Next-gen GABA modulators promise benzo benefits without the baggage. They’re in the pipeline, aiming to calm brains smarter and safer.
FDA Warnings and Updated Guidelines on Benzodiazepine Use
The FDA’s clear: benzos work, but beware. Updated 2025 guidelines flag misuse risks, even at normal doses. Mixing with opioids is a red line—respiratory depression can kill. Clinicians are urged to weigh benefits against hazards carefully.
It’s a balancing act. Benzos have a role, but caution’s the watchword.
Alternative Treatments for Insomnia and Daytime Anxiety
If benzos are out, what’s in? For insomnia, z-drugs, sedating antidepressants like trazodone, or orexin blockers like suvorexant step up. Daytime anxiety might lean on SSRIs or mindfulness, dodging benzo pitfalls.

These swaps keep treatment moving without leaning on risky crutches.
Cautionary Use in PTSD and Substance Abuse Comorbidity
PTSD and substance abuse are red flags for benzos. Studies show they might worsen fear processing or fuel addiction, especially post-trauma. A 2025 meta-analysis found clonazepam no better than placebo for PTSD nightmares—and maybe harmful.
For these patients, alternatives like therapy or newer meds are safer bets.
Q&A Section
Q: How does ketamine compare to traditional antidepressants for TRD?
A: Ketamine’s a speedster—relief can hit in hours, not weeks like SSRIs or SNRIs. It targets glutamate, not serotonin, offering a fresh angle when standard meds fail. But it’s not a solo act; effects may fade, needing repeat doses, and it requires clinic visits. Traditional antidepressants are slower but simpler to manage long-term. For TRD, ketamine’s edge is its rapid punch, though it’s best paired with a broader plan.
Conclusion
Treatment-resistant depression is a beast, but hope’s not lost. Ketamine for treatment-resistant depression is rewriting the script, offering fast relief where others stall. Add in alternatives like trazodone or suvorexant, and the toolbox grows. At BrainTalking, we see a future where research—GABA drugs, tailored therapies—meets patients’ needs head-on. For now, blending meds, therapy, and support is the path forward.

- TRD resists standard antidepressants, affecting 30% of depression cases.
- Ketamine treatment for resistant depression acts fast via glutamate, unlike slower SSRIs.
- Anxiety often tags along with TRD, complicating care—alternatives like mirtazapine help.
- Future treatments, from GABA modulators to PTSD-specific drugs, promise better options.




