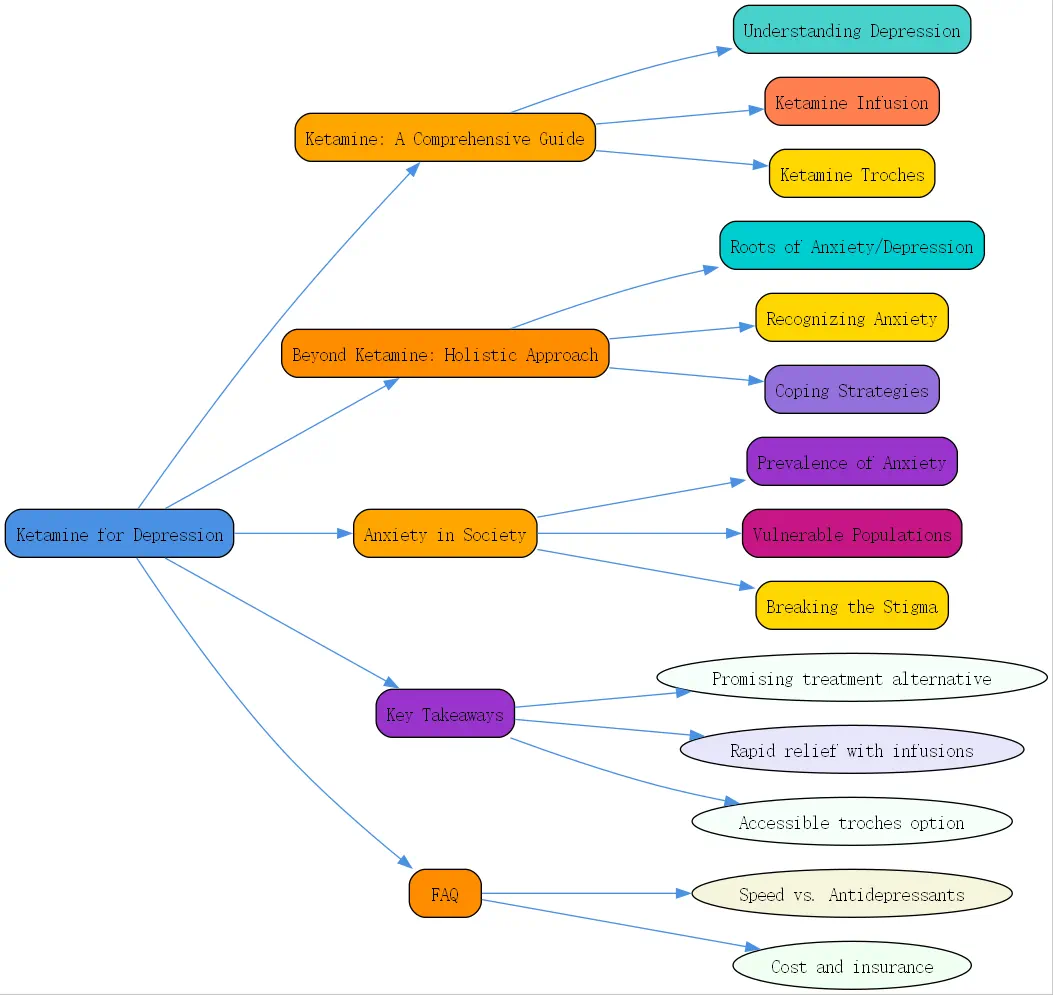
Ketamine for Depression: A Comprehensive Guide
Depression can feel like an overwhelming weight that’s impossible to escape. For many individuals, traditional treatments provide limited relief, leaving them searching for more effective alternatives. In recent years, ketamine has emerged as a promising option for those struggling with persistent depression. This comprehensive guide explores how ketamine for depression works, the different administration methods, and important considerations for those contemplating this treatment path.
Understanding Depression and Current Treatment Limitations
Depression is not merely feeling sad—it’s a chronic condition that requires effective management strategies. Many individuals describe it as an ongoing battle that affects every aspect of daily life. As one patient shares, “”It’s a chronic thing I have to manage,”” highlighting the persistent nature of depression that conventional treatments sometimes fail to address adequately.
Traditional antidepressants such as SSRIs (selective serotonin reuptake inhibitors), SNRIs (serotonin-norepinephrine reuptake inhibitors), and tricyclics have been the standard first-line treatments for decades. However, their effectiveness is surprisingly limited, with research indicating only about a 33% success rate. This means two-thirds of patients may not receive adequate relief from these conventional medications, leaving a significant treatment gap.
The journey toward mental health often begins with acknowledgment and acceptance. Many people report that recognizing their condition was a crucial first step: “”One of the biggest steps I’ve taken in healing and effectively managing my anxiety is the acknowledgment and the acceptance that it’s there and that it’s a part of who I am.”” This mindset shift creates the openness needed to explore alternative treatments like ketamine.
Ketamine Infusion for Depression: A Novel Approach

Ketamine, originally developed as an anesthetic, has gained attention for its remarkable antidepressant properties. Unlike traditional antidepressants that may take weeks to show effects, ketamine infusions can provide rapid relief, sometimes within hours or days. This swift action makes it particularly valuable for those experiencing severe depression or suicidal thoughts.
The science behind ketamine’s effectiveness lies in its unique mechanism of action. While conventional antidepressants focus on serotonin, norepinephrine, or dopamine, ketamine primarily works through the glutamate system—the brain’s most abundant excitatory neurotransmitter. By modulating NMDA receptors, ketamine triggers a cascade of events that ultimately promotes neuronal growth and connectivity.
Clinical studies on ketamine infusions for depression show impressive results. According to research, ketamine demonstrates a 70-80% success rate—more than double that of traditional antidepressants. As one medical professional noted, “”When you’ve got a traditional treatment such as SSRIs or SNRIs or tricyclics that your first-line therapy has about a 33% success rate, ketamine most of the research shows us 70 to 80% success rate.””

Perhaps most fascinating is ketamine’s role in neuroplasticity—the brain’s ability to form new neural connections. This “”rewiring”” capability helps explain why ketamine’s effects can persist beyond the immediate treatment period. As one expert explains, “”Using my mind in a certain way can actually change how the brain functions and also physically how the brain is.”” This neuroplasticity effect may be key to ketamine’s sustained antidepressant benefits.
Ketamine Troches for Depression: An Alternative Option
While ketamine infusions receive much attention, ketamine troches (pronounced “”tro-keys””) offer another administration method worth considering. These dissolvable lozenges are placed under the tongue, allowing the medication to be absorbed through the oral mucosa. BrainTalking specialists note that troches provide a more accessible and potentially more affordable alternative to infusions.
Ketamine troches differ from infusions in several important ways. Infusions deliver ketamine directly into the bloodstream, resulting in higher bioavailability and more controlled dosing. Troches, however, offer greater convenience as they can often be administered at home after proper medical assessment and instruction. The absorption rate and bioavailability are lower than with infusions, so dosages typically need adjustment accordingly.
When comparing ketamine troches versus ketamine infusions for depression, several factors come into play. Infusions generally provide more intense and immediate effects, making them potentially more suitable for severe depression cases. Troches, on the other hand, may be preferable for maintenance therapy after a successful infusion series or for patients with milder symptoms who prefer a less intensive approach.
The Ketamine Experience: What to Expect
Many patients wonder what actually happens during ketamine treatment. The experience is often described as dissociative—a temporary feeling of detachment from one’s normal reality. As one patient characterized it, “”It’s not a true psychedelic but it’s a psychedelic-like experience”” where “”they’re awake, they’re just in this disassociated space.””
This altered state of consciousness can facilitate emotional processing and healing, particularly for trauma-related depression. Patients often report gaining new perspectives on past traumatic experiences: “”I would watch what happened to me in my trauma event through multiple of them and then basically at the end I would see that okay in the end the only thing that mattered is how I responded to it then and after and that I made it out safe.”” This reframing process can be profoundly therapeutic.
Integration is a crucial aspect of ketamine treatment. The insights gained during sessions can be powerful but may require professional guidance to fully process and incorporate into daily life. Many providers recommend combining ketamine treatment with talk therapy to maximize benefits. This integration helps patients translate their ketamine experiences into lasting positive changes in thought patterns and behaviors.
Combining Ketamine with Other Treatments for Optimal Results
Research consistently shows that combined therapeutic approaches yield the best outcomes for depression treatment. As one healthcare provider states, “”Combined methods of treatment tend to be more effective in managing anxiety. All the literature would say that the best treatment for all psychiatric conditions but particularly depression and anxiety is the combination of therapy with medication.””
Mindfulness practices complement ketamine therapy particularly well. Meditation, deep breathing exercises, and present-moment awareness techniques help patients maintain the neural changes initiated by ketamine treatment. These practices encourage continued neuroplasticity and provide practical tools for managing day-to-day stressors that could otherwise trigger depressive episodes.
The development of personalized coping strategies is essential for long-term well-being. As one expert points out, “”Coping skills are really hobbies and they’re not something where you can one size fit all everybody.”” Some individuals find relief through creative expression, physical activity, time in nature, or social connection. The goal is to discover what specifically works for each individual’s unique circumstances and preferences.
Is Ketamine Right for You? Considerations and Precautions
While ketamine for depression shows promise, it’s not without potential side effects. During treatment, patients may experience temporary dissociation, dizziness, nausea, or increased blood pressure. These effects typically resolve quickly after each session. Long-term or frequent use requires careful monitoring as research on extended ketamine treatment is still developing.
Finding a qualified ketamine provider is essential for safe and effective treatment. BrainTalking recommends seeking practitioners with specific training in ketamine administration for mental health conditions, preferably with backgrounds in psychiatry, anesthesiology, or pain management. A thorough evaluation should occur before beginning treatment, including a comprehensive review of medical history and current medications.
Proper screening for anxiety and other mental health conditions is crucial before starting ketamine treatment. Many depression cases co-occur with anxiety disorders, which may influence how patients respond to ketamine. A health task force now recommends anxiety screening for all adults under 65, acknowledging that “”anxiety is associated with a number of other problems such as substance use disorders or substance misuse and obviously that’s got a cascade of problems.””
Beyond Ketamine: Addressing Anxiety and Depression Holistically
Understanding the Roots of Anxiety and Depression
Depression and anxiety rarely have single causes. Instead, they typically result from a complex interplay of biological, genetic, and environmental factors. As one mental health professional explains, “”Anxiety most mental health conditions is multifactorial in its cause, meaning that there is a pretty significant biologic component. There’s also a genetic component, meaning that if your mom had anxiety you might also have anxiety, and then of course people can be triggered to have anxiety by life events.””
Many individuals with depression also experience anxiety, particularly those with histories of trauma or PTSD. The symptoms often feed into each other: “”Everything at PTSD feeds on another. So if you’re not sleeping it directly affects two or three attributes or behaviors downstream, and if you are in that fight you fight about everything.”” This interconnection highlights the importance of comprehensive treatment approaches.
Interestingly, some individuals have found ways to reframe their anxiety as a potential asset. One person described anxiety as “”a superpower for me. It allows me to think very hypercritical, it allows me to see the big picture.”” This perspective shift can help reduce shame and stigma while acknowledging the very real challenges of living with anxiety and depression.
Recognizing Anxiety: Symptoms and Diagnosis
Anxiety often manifests physically in ways many people don’t initially associate with a mental health condition. Common physical symptoms include heart palpitations, muscle tension, headaches, digestive issues, and even chronic pain. As one sufferer described, “”It manifests itself in the physical form 100 percent. My heart will start beating out of my chest, even just the feeling of being numb or frozen in time.””
The emotional toll of anxiety includes overwhelming worry, panic, feelings of impending doom, shame, and persistent unworthiness. Many report a sense of being trapped in their own thoughts: “”It is constant thinking. My brain doesn’t shut down well no matter what, and that’s just where my thoughts just run away from me.”” These symptoms can significantly impact quality of life.
When anxiety begins to interfere with daily functioning, it’s typically considered clinically significant. Many report difficulties with social interactions, work performance, and even basic activities: “”I wouldn’t get up in the morning ready to conquer the world… I didn’t do really well around people in social situations, would get very overwhelmed and very panicky and would try to find a way to escape.”” These functional impairments often prompt individuals to seek help.
Coping Strategies for Managing Anxiety and Depression
Therapy provides a structured environment to develop personalized coping strategies and process difficult emotions. Although hesitation is common, many find therapy invaluable: “”I was very resistant to pursue medication as an option as that goes for talk therapy as well, but I’ve come to lean on both of those tools in addition to my meditation practice to support my healing and just taking care of myself.””
Medication plays an important role for many patients, including those receiving ketamine treatments. While ketamine may address the underlying neurobiology of depression, traditional antidepressants or anti-anxiety medications might still be beneficial for symptom management. The right medication approach varies widely between individuals and often requires adjustment over time.
Mindfulness and meditation techniques offer powerful tools for managing anxiety symptoms. These practices help interrupt rumination cycles and bring awareness to the present moment. Regular practice appears to strengthen the neurological pathways that support emotional regulation: “”This meditation helped manage stress… just taking care of myself.””
The Broader Context: Anxiety in Society
Prevalence of Anxiety: A Growing Concern
Anxiety disorders represent the most common mental health conditions in America, affecting millions of people across all demographics. Their prevalence appears to be increasing, potentially driven by factors like digital connectivity, economic pressures, and changing social dynamics. The ubiquity of anxiety makes treatment options like ketamine for depression and anxiety increasingly relevant.
Societal expectations and chronic stress contribute significantly to anxiety levels. Many people report feeling pressure to maintain impossible standards of productivity, success, or personal appearance. These expectations can create a perpetual state of feeling inadequate or behind, fueling anxiety and depression in vulnerable individuals.
Vulnerable Populations and Anxiety
Research indicates that women experience anxiety disorders at approximately twice the rate of men. This disparity likely stems from both biological factors and societal influences. As one woman noted, “”The expectations that is put into a woman’s space creates that anxiety. It creates that constant ongoing of thinking of emotions and things that we have to deal with day to day, but again it goes also back to the science and how our body works. We are just crafted to be emotional creatures.””
Studies suggest that Black adults are 20% more likely to experience depression and anxiety compared to other demographic groups. This disparity reflects both healthcare access issues and the impact of specific stressors like discrimination and systemic inequities. Cultural factors may also influence how symptoms are expressed and whether individuals seek professional help.
Breaking the Stigma: Seeking Help and Supporting Others
Early screening and treatment can significantly improve outcomes for those with depression and anxiety. Recent health guidelines now recommend universal anxiety screening for adults under 65, recognizing that early intervention prevents more severe complications. This shift represents an important step toward normalizing mental health care as part of routine health maintenance.
Open conversations about mental health help reduce stigma and encourage treatment-seeking. Many report that sharing their experiences was transformative: “”Not holding those feelings in was one of the better things for me.”” By speaking openly about conditions like depression and treatments like ketamine for depression, we create space for others to seek help without shame.
Supporting someone with depression or anxiety requires patience, empathy, and understanding. Many patients express the importance of having people who acknowledge their struggles without judgment: “”Every now and then I may not be on the top of my game and I just need that reciprocity just to understand that there’s something going on and just give me the help I need.””
Takeaways About Ketamine for Depression
- Ketamine offers a promising alternative for depression treatment with a 70-80% success rate compared to traditional antidepressants’ 33% success rate
- Ketamine infusions for depression provide rapid relief, sometimes within hours, making them valuable for severe cases
- Ketamine troches represent a more accessible alternative to infusions, potentially suitable for maintenance therapy
- The most effective approach combines ketamine with talk therapy, mindfulness practices, and personalized coping strategies
- Proper screening and qualified providers are essential for safe, effective ketamine treatment
- The dissociative experience during ketamine treatment may facilitate emotional processing and healing from trauma
- Ketamine’s ability to promote neuroplasticity helps explain its lasting benefits beyond the immediate treatment period
Frequently Asked Questions
How quickly does ketamine work for depression compared to traditional antidepressants?
Unlike traditional antidepressants that typically take 4-6 weeks to show full effects, ketamine infusions for depression can produce significant improvement within hours to days of treatment. Many patients report noticeable mood elevation after their first or second infusion. This rapid action makes ketamine particularly valuable for those experiencing severe depression or suicidal thoughts where immediate relief is crucial. However, the sustainability of these effects often requires a series of treatments and possibly maintenance sessions. BrainTalking specialists recommend a comprehensive treatment plan that accounts for both immediate relief and long-term management.




