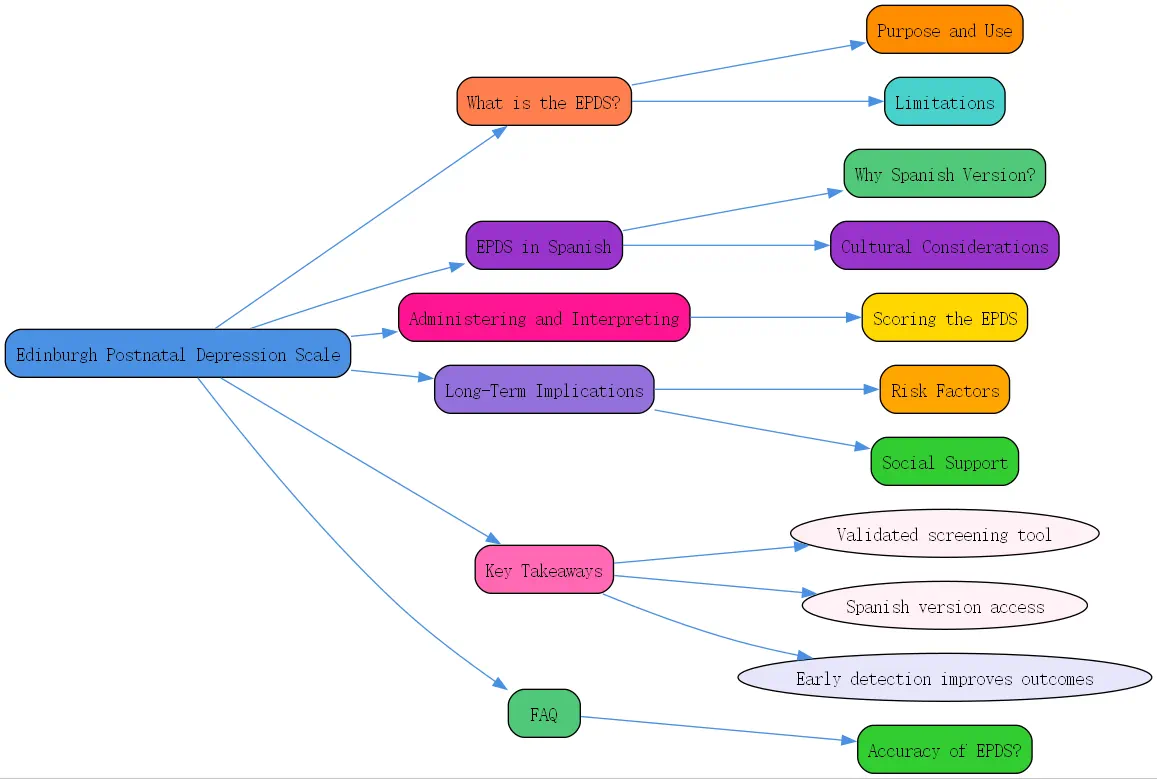
What is the Edinburgh Postnatal Depression Scale (EPDS)?
The Edinburgh Postnatal Depression Scale (EPDS) is a widely recognized screening tool designed specifically to detect symptoms of depression in women during the postnatal period. Developed in the 1980s by researchers in Edinburgh, Scotland, this 10-question self-report questionnaire has become a cornerstone in maternal mental health assessment worldwide.
The EPDS focuses on emotional symptoms rather than physical symptoms that might be common during the postpartum period, such as fatigue or changes in sleep patterns, which could be confused with normal postpartum experiences. This targeted approach makes it particularly effective at identifying women who may be experiencing postnatal depression without relying on symptoms that naturally occur after childbirth.
Unlike general depression screening tools, the Edinburgh Postnatal Depression Scale was designed with the unique experiences of new mothers in mind. It can identify symptoms that might otherwise be overlooked during routine check-ups, providing healthcare providers with valuable insights into a mother’s emotional wellbeing during what can be a vulnerable time.
Purpose and Use of the EPDS
The primary purpose of the EPDS is to screen for postnatal depression, allowing for early identification and intervention. Early detection is crucial as untreated postnatal depression can have serious implications for both mother and child. It can affect maternal-infant bonding, child development, and family dynamics.
Healthcare providers often administer the EPDS during routine postpartum check-ups, typically between 6-12 weeks after childbirth. However, the tool can be used at multiple time points throughout the first year following birth, allowing for continued monitoring of a mother’s mental health. The EPDS can also be used during pregnancy to identify women at risk of developing postnatal depression.
The EPDS serves as a conversation starter, opening the door for healthcare providers to discuss mental health concerns that mothers might otherwise be reluctant to bring up due to stigma or shame. This dialog can lead to appropriate referrals for further assessment and treatment when necessary.
Who Should Use the EPDS?
The Edinburgh Postnatal Depression Scale is intended for use by various healthcare professionals who work with postpartum women. This includes obstetricians, gynecologists, midwives, pediatricians, family physicians, public health nurses, and mental health professionals specializing in maternal health.
All new mothers should be screened using the EPDS, regardless of their background or risk factors. Universal screening helps identify women who may not outwardly display symptoms or who may be hesitant to discuss their emotional struggles. This approach ensures that no mother falls through the cracks of the healthcare system when it comes to mental health support.
Women with a history of depression or other mental health conditions should receive particular attention, as they face an increased risk of developing postnatal depression. The same applies to mothers facing additional stressors such as financial difficulties, lack of social support, or complications during pregnancy or delivery.
Limitations of the EPDS
While the Edinburgh Postnatal Depression Scale is an excellent screening tool, it does have certain limitations that healthcare providers should be aware of. First and foremost, the EPDS is not a diagnostic tool. A high score indicates the possible presence of depression but does not constitute a clinical diagnosis. Further assessment by qualified mental health professionals is necessary for an accurate diagnosis.
The EPDS focuses primarily on depressive symptoms and may not adequately capture other perinatal mood disorders, such as anxiety disorders or postpartum psychosis. Women experiencing these conditions might score below the threshold on the EPDS while still requiring mental health support.
Cultural factors can influence how women interpret and respond to the questions on the EPDS. What constitutes “”feeling sad”” or “”crying”” may vary across cultures, potentially affecting the tool’s sensitivity and specificity. This is why cultural adaptations of the scale, such as the Spanish Edinburgh Postnatal Depression Scale, are so valuable.

Edinburgh Postnatal Depression Scale in Spanish
For Spanish-speaking mothers, having access to the Edinburgh Postnatal Depression Scale in their native language is crucial for accurate assessment of their mental health. The Spanish edinburgh postnatal depression scale (Escala de Depresión Postnatal de Edimburgo) maintains the integrity of the original tool while accounting for linguistic and cultural nuances.
The Spanish translation has been validated in numerous studies across different Spanish-speaking populations, making it a reliable tool for healthcare providers working with Hispanic and Latina mothers. This validation process ensures that the Spanish EPDS measures the same psychological constructs as the original version with comparable accuracy.
At BrainTalking, we recognize that language should never be a barrier to receiving appropriate mental health care, especially during the vulnerable postpartum period. The availability of the Spanish edinburgh depression scale represents an important step toward equitable maternal mental health services.
Why Use a Spanish Version of the EPDS?
Using the edinburgh postnatal depression scale spanish version offers numerous benefits for both healthcare providers and Spanish-speaking mothers. Language barriers can significantly impact the accuracy of mental health assessments. When mothers cannot fully understand the questions being asked, their responses may not accurately reflect their emotional state, leading to missed opportunities for intervention.
The Spanish EPDS allows mothers to express their feelings in the language they’re most comfortable with, resulting in more honest and accurate responses. This is particularly important when discussing sensitive mental health topics that require nuanced language to describe emotional experiences.
In the United States, where the Hispanic population continues to grow, having the edinburgh postnatal depression scale in Spanish is essential for providing culturally responsive care. This adaptation acknowledges the importance of linguistic and cultural competence in healthcare and demonstrates respect for cultural diversity.
Accessing the Spanish Edinburgh Postnatal Depression Scale
The Spanish edinburgh postnatal depression scale is widely available through various channels. Healthcare organizations, hospitals, clinics, and public health departments typically have access to validated Spanish translations of the EPDS. These can be obtained from professional organizations focused on maternal mental health or directly from the original publishers with appropriate permissions.
Digital versions of the Spanish EPDS are increasingly available through electronic health record systems and maternal health apps. This technological integration makes it easier for healthcare providers to incorporate the tool into routine care, even in settings where printed materials in multiple languages might be limited.
BrainTalking provides resources for healthcare professionals seeking to implement the Spanish edinburgh depression scale in their practice. We offer guidance on proper administration and scoring to ensure that the tool is used effectively across diverse healthcare settings.
Cultural Considerations When Using the Spanish EPDS
When administering the Spanish Edinburgh Postnatal Depression Scale, healthcare providers should be aware of important cultural considerations that may influence how mothers respond to the questions. Hispanic cultures often have unique perspectives on motherhood, mental health, and emotional expression that may affect how women interpret and answer the questions on the EPDS.

The concept of “”marianismo”” in some Hispanic cultures, which idealizes maternal sacrifice and strength, may make some women reluctant to acknowledge feelings of sadness or inability to cope. Understanding these cultural values helps providers create a safe space where mothers feel comfortable expressing vulnerability without fear of judgment.
Family involvement is often central in Hispanic cultures, with extended family members playing significant roles in childcare and support. Questions about coping and social support may need contextual understanding, as mothers may rely heavily on family networks rather than professional services for assistance.
Administering and Interpreting the Edinburgh Postnatal Depression Scale
Proper administration and interpretation of the EPDS are essential for its effectiveness as a screening tool. Whether using the original English version or the Spanish edinburgh postnatal depression scale, following standardized procedures ensures reliable results.
The tool’s simplicity is one of its greatest strengths, making it accessible to busy healthcare providers and easy for mothers to complete. Despite this simplicity, the information gathered can provide valuable insights into a mother’s emotional wellbeing during the challenging postpartum period.
When introducing the EPDS to mothers, healthcare providers should explain its purpose in a non-stigmatizing way, emphasizing that emotional challenges are common after childbirth and that honest answers will help ensure appropriate support. This approach helps normalize the screening process and encourages candid responses.
Step-by-Step Guide to Administering the EPDS
Administering the Edinburgh Postnatal Depression Scale involves several key steps to ensure accuracy and effectiveness. First, select an appropriate time and setting for the screening. The environment should be private, comfortable, and free from distractions to allow mothers to focus on their responses.
Explain the purpose of the screening tool in simple terms, emphasizing that it’s a routine part of postpartum care designed to help ensure the mother’s wellbeing. Stress that there are no right or wrong answers and that honesty is important for getting appropriate support.
Provide clear instructions for completing the questionnaire, explaining that each question refers to how the mother has felt over the past seven days, not just on the day of the screening. This timeframe is important for capturing a representative picture of her emotional state rather than a momentary mood.
Scoring the Edinburgh Postnatal Depression Scale
Scoring the EPDS is straightforward but requires attention to detail. Each of the 10 questions on the edinburgh postnatal depression scale is scored on a scale of 0-3, with the total score ranging from 0-30. Questions 1, 2, and 4 are scored from 0-3, while questions 3 and 5-10 are reverse-scored (3-0).
Healthcare providers should calculate the total score immediately after the mother completes the questionnaire. This allows for prompt discussion of the results and implementation of follow-up plans if necessary. Digital tools and apps can assist with accurate scoring and record-keeping.
Documentation of EPDS scores in the mother’s medical record is important for tracking changes over time and ensuring continuity of care. Many electronic health record systems now include templates for recording EPDS scores along with relevant clinical notes about the mother’s presentation and any follow-up actions taken.
Understanding EPDS Cut-off Scores and Interpretation
The interpretation of EPDS scores relies on established cut-off points that indicate the likelihood of depression. Generally, a score of 10 or higher suggests possible depression, while a score of 13 or higher indicates likely depression requiring further assessment. For the Spanish edinburgh depression scale, these cut-off points may vary slightly based on validation studies in specific populations.
It’s crucial to note that the EPDS includes item 10, which specifically addresses thoughts of self-harm. Any positive response to this question (score greater than 0) requires immediate attention and risk assessment, regardless of the total score. Safety planning should take precedence in these situations.
When discussing EPDS results with mothers, healthcare providers should use supportive, non-judgmental language. Framing high scores as an opportunity to receive appropriate support rather than as a personal failure helps reduce stigma and encourages engagement with recommended follow-up care.
Long-Term Implications of Mental Health in Postnatal Mothers
Untreated postnatal depression can have far-reaching consequences for mothers, children, and families. Research consistently shows that maternal depression can affect infant attachment, cognitive development, and emotional regulation. Children of mothers with untreated postnatal depression may face increased risks of developmental delays and behavioral problems.
Early identification through tools like the Edinburgh Postnatal Depression Scale, followed by appropriate intervention, can significantly improve outcomes. Effective treatments for postnatal depression include psychotherapy, medication when appropriate, support groups, and lifestyle modifications to support mental wellbeing.
BrainTalking emphasizes the importance of a comprehensive approach to maternal mental health that extends beyond the immediate postpartum period. Ongoing support and monitoring throughout the first year after childbirth can help address evolving mental health needs as mothers navigate the challenges of parenthood.
Potential Risk Factors and Adverse Mental Health Outcomes
Several factors increase a woman’s risk of developing postnatal depression, including a history of depression or anxiety, limited social support, relationship difficulties, stressful life events during pregnancy or early postpartum, and pregnancy or birth complications. Understanding these risk factors helps healthcare providers identify women who may benefit from more frequent screening and preventive interventions.
Adverse mental health outcomes extend beyond depression to include anxiety disorders, post-traumatic stress disorder related to childbirth, and in rare cases, postpartum psychosis. The EPDS may detect some anxiety symptoms but is primarily designed for depression screening. Comprehensive mental health assessment should consider the full spectrum of potential conditions.
The COVID-19 pandemic has introduced additional stressors for new mothers, including increased isolation, financial strain, and healthcare access challenges. These factors may exacerbate existing risk factors for postnatal depression, highlighting the importance of consistent screening and support during this time.
Effects of Loss and Grief on Mental Well-being
Loss and grief can significantly impact maternal mental health. This includes pregnancy loss, birth trauma, loss of the idealized birth experience, or grief related to the changes in identity and lifestyle that accompany motherhood. These experiences can contribute to or complicate postnatal depression.
Healthcare providers should be sensitive to these grief reactions when interpreting EPDS results. A high score on the edinburgh postnatal depression scale may reflect a normal grief response to loss rather than clinical depression in some cases, though both deserve attention and support.
For mothers experiencing grief alongside depression, integrated treatment approaches that address both the grief process and depressive symptoms are most effective. This might include grief counseling alongside traditional depression treatments like cognitive-behavioral therapy or interpersonal therapy.
Importance of Social Support and Clear Communication
Strong social support networks serve as protective factors against postnatal depression. Partners, family members, friends, and community connections all play vital roles in supporting new mothers. Healthcare providers should assess a mother’s support system when evaluating mental health risks and develop plans to strengthen these networks when needed.
Clear communication between healthcare providers and mothers is essential for effective mental health care. This includes explaining the purpose and results of screening tools like the Spanish edinburgh postnatal depression scale in accessible language, providing transparent information about treatment options, and maintaining open lines of communication throughout the recovery process.
Support groups specifically designed for mothers experiencing postnatal depression can provide both practical assistance and emotional validation. These groups are particularly valuable for mothers who may feel isolated or misunderstood in their struggles, offering connection with others facing similar challenges.
Key Takeaways
- The Edinburgh Postnatal Depression Scale is a validated screening tool for detecting postnatal depression symptoms in new mothers.
- The Spanish edinburgh postnatal depression scale provides essential access to mental health screening for Spanish-speaking mothers.
- Proper administration and interpretation of the EPDS require attention to scoring details and established cut-off points.
- Cultural considerations are important when using the edinburgh postnatal depression scale spanish version with diverse populations.
- Early detection and intervention for postnatal depression can significantly improve outcomes for mothers, children, and families.
- Social support, clear communication, and comprehensive follow-up care are essential components of effective maternal mental health services.
Frequently Asked Questions
How accurate is the Edinburgh Postnatal Depression Scale in identifying women with postnatal depression?
The EPDS has been extensively validated and shows good sensitivity and specificity for detecting postnatal depression. Studies indicate that the tool correctly identifies approximately 86% of women with postnatal depression (sensitivity) and correctly identifies about 78% of women without depression (specificity). These rates may vary slightly for the Spanish edinburgh postnatal depression scale depending on the specific population.




