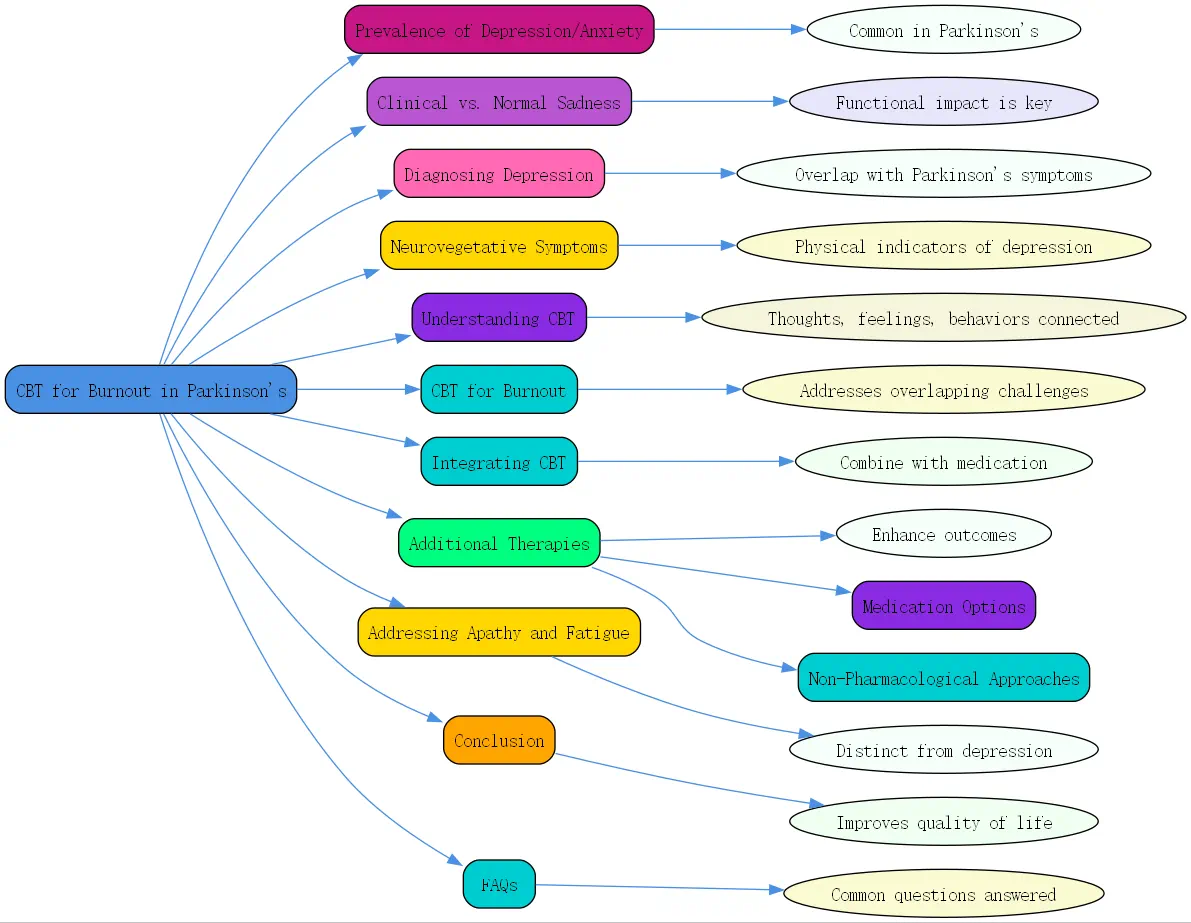
The Prevalence of Depression and Anxiety in Parkinson’s Disease
Depression and anxiety are significantly more prevalent in individuals with Parkinson’s disease compared to the general population. This elevated occurrence isn’t merely a psychological reaction to having a chronic condition but has biological underpinnings related to the disease itself. Parkinson’s affects not only dopamine levels but also disrupts other crucial neurotransmitters like serotonin and norepinephrine, which play vital roles in mood regulation.
According to experts, approximately 25% of people with Parkinson’s will experience a major depressive episode at some point during their illness. Perhaps more concerning is that at least half will encounter mood symptoms significant enough to impact their daily functioning, even if these symptoms don’t meet the full criteria for major depression.
“”Mood disturbances are over-represented in Parkinson’s compared to the general population for several biological reasons,”” explains neuropsychiatry specialists. The disease’s effect on multiple neurotransmitter systems creates a complex neurochemical environment where mood disorders can flourish.
An interesting clinical observation is that anxiety frequently accompanies depression in Parkinson’s patients. In fact, the co-occurrence is so common that medical professionals recommend screening for anxiety whenever depression is suspected. About half of all Parkinson’s patients experience clinically significant anxiety symptoms at some point, with full-blown anxiety disorders affecting approximately one-third of individuals living with the condition.
Differentiating Clinical Depression/Anxiety from Normal Sadness
One of the most crucial distinctions to understand is the difference between clinical depression or anxiety and the natural emotional responses to being diagnosed with Parkinson’s disease. While it’s entirely normal to feel sad, worried, or demoralized about having a progressive neurological condition, clinical depression and anxiety represent something fundamentally different.
The key differentiator is functional impact. When sadness or worry crosses the line into interfering with your ability to complete day-to-day activities, it likely indicates a clinical disorder requiring treatment. Similar to how cognitive behavioral therapy for depression helps identify these distinctions, understanding the threshold between normal emotional responses and clinical disorders is essential.
“”When you’re depressed or anxious to the point where you’re actually not completing your day-to-day activities, that’s when it crosses the line and becomes a clinical disorder,”” notes mental health professionals working with Parkinson’s patients. This distinction acknowledges the biological basis of these mood disorders in the context of Parkinson’s.
Much like Parkinson’s motor symptoms require medication to improve, depression and anxiety associated with Parkinson’s often need biological intervention through appropriate medications. However, this doesn’t diminish the importance of cognitive behavioral therapy for anxiety and other psychological approaches. A comprehensive treatment approach incorporates both biological and psychological interventions.
Diagnosing Depression: Distinguishing from Parkinson’s Symptoms
Diagnosing depression in Parkinson’s patients presents unique challenges because many symptoms overlap with the disease itself. How does one determine whether symptoms like fatigue, poor sleep, or reduced appetite stem from depression or are simply manifestations of Parkinson’s?
This clinical dilemma requires careful assessment. Depression is diagnosed as a syndrome, typically requiring five or more symptoms to meet the threshold for a major depressive disorder. While sad mood is often present, it’s important to note that depression can exist without overt sadness. Loss of motivation or interest in previously enjoyable activities (anhedonia) may be the predominant feature.
“”You don’t necessarily need to be sad or tearful to have depression,”” emphasize psychiatric experts. “”Just losing your motivation or interest in things is sufficient.””
Other significant indicators include feelings of guilt, hopelessness, and thoughts that life isn’t worth living. These symptoms aren’t typical of mere demoralization and warrant clinical attention. In severe cases, suicidal thoughts may emerge, representing a serious warning sign requiring immediate intervention.

Cognitive behavioral therapy for burnout can be particularly helpful in addressing these symptoms by teaching patients to recognize and challenge negative thought patterns that contribute to depressive thinking. Through structured approaches, cognitive behavioral therapy helps individuals develop more balanced perspectives and effective coping strategies.
Neurovegetative Symptoms: Indicators of Depression
Beyond the emotional aspects of depression, there are physical manifestations known as neurovegetative symptoms that can help clinicians distinguish depression in Parkinson’s patients. These symptoms often serve as objective markers that aid in accurate diagnosis.
Psychomotor slowing represents one such symptom. While Parkinson’s causes bradykinesia (slowness of movement), depression can exacerbate this with additional cognitive slowing. Clinicians may notice speech latency—a delay between being asked a question and responding—which is characteristic of moderate to severe depression.
Sleep disturbances present another common indicator. While sleep problems frequently occur in Parkinson’s, specific patterns of sleep disruption can signal depression. Similarly, appetite changes occur in both conditions, but depression may cause either significant appetite loss or, in atypical cases, increased eating as a form of emotional self-soothing.
Cognitive impairment represents perhaps the most concerning overlap. Depression can cause such profound concentration and memory problems that it mimics dementia. The encouraging news is that cognitive behavioral therapy for burnout, alongside appropriate medication, can often reverse these cognitive effects when they stem from depression rather than neurodegenerative changes.
Understanding Cognitive Behavioral Therapy (CBT)

Cognitive Behavioral Therapy (CBT) stands as one of the most evidence-based psychological treatments for various mental health conditions, including depression and anxiety. For individuals dealing with Parkinson’s disease, a cognitive behavioral therapy approach can provide valuable tools for managing the psychological aspects of their condition.
At its core, CBT is based on the premise that our thoughts, feelings, and behaviors are interconnected. By identifying and challenging distorted thinking patterns, individuals can change negative emotional responses and develop healthier behavioral patterns. This structured, goal-oriented therapy typically focuses on present issues rather than delving deeply into past experiences.
“”CBT teaches patients to recognize automatic negative thoughts and replace them with more balanced, realistic alternatives,”” explains mental health professionals. “”This process can be particularly helpful for individuals experiencing depression or anxiety alongside Parkinson’s disease.””
A cognitive behavioral therapy for anxiety specifically targets fear-based thoughts and physiological responses. Through techniques like cognitive restructuring, exposure therapy, and relaxation training, patients learn to manage anxiety symptoms that often accompany Parkinson’s. In managing social anxiety a cognitive behavioral therapy approach client workbook, therapists outline specific strategies to help individuals facing social anxiety alongside their neurological symptoms.
Similarly, cognitive behavioral therapy for depression helps patients identify and challenge depressive thought patterns that contribute to low mood. This approach has shown particular efficacy in addressing the unique combination of physical and psychological challenges faced by Parkinson’s patients.
How Cognitive Behavioral Therapy for Burnout Can Help
Burnout—characterized by emotional exhaustion, cynicism, and reduced efficacy—frequently accompanies chronic conditions like Parkinson’s disease. The constant strain of managing physical symptoms, medication schedules, and lifestyle adjustments can deplete psychological resources, leading to burnout that compounds existing depression and anxiety.
Cognitive behavioral therapy for burnout offers a structured approach to addressing these overlapping challenges. By teaching patients to recognize early warning signs of burnout and implement strategic interventions, CBT helps prevent the downward spiral that can lead to more severe depression or anxiety.
“”One of the strengths of CBT is its focus on developing practical coping skills,”” notes BrainTalking’s psychology experts. “”For Parkinson’s patients experiencing burnout, these skills can make the difference between feeling overwhelmed and maintaining a sense of control.””
CBT provides strategies for energy conservation, setting realistic goals, and prioritizing activities to accommodate fluctuating symptom severity. These approaches help patients manage fatigue—a symptom common to both Parkinson’s and depression—more effectively.
Sleep issues, another overlapping symptom, respond particularly well to specific CBT techniques. Cognitive behavioral therapy for insomnia components can be integrated into treatment plans, helping patients establish healthier sleep patterns despite the disruptions caused by their neurological condition.
Integrating Cognitive Behavioral Therapy
The most effective approaches to managing depression and anxiety in Parkinson’s disease typically involve combining cognitive behavioral therapy with appropriate medication. This integrated approach addresses both the biological and psychological aspects of mood disorders.
Medication may target the neurotransmitter imbalances contributing to depression and anxiety, while CBT provides the psychological tools to modify thought patterns and behaviors that maintain negative mood states. Research consistently demonstrates that this combination approach yields better outcomes than either treatment alone.
“”The integration of pharmaceutical and psychological approaches represents the gold standard in treating mood disorders in Parkinson’s patients,”” explains mental health specialists. This comprehensive strategy acknowledges the complex interplay between neurological and psychological factors in Parkinson’s disease.
Beyond formal therapy, lifestyle modifications support and extend the benefits of cognitive behavioral therapy. Regular exercise, social engagement, stress management techniques, and dietary considerations all contribute to improved mood and reduced symptom burden. These adjustments align with CBT principles by creating environments and routines that support psychological well-being.
BrainTalking recommends that patients work with healthcare providers to develop personalized treatment plans that incorporate medication, therapy, and lifestyle modifications in proportions suitable to their unique needs and preferences.
Additional Therapies for Depression & Anxiety Associated with Parkinson’s
While cognitive behavioral therapy and medication form the cornerstone of treatment for mood disorders in Parkinson’s, several additional approaches can enhance outcomes and quality of life.
Medication Options for Managing Mood Disorders
Selective Serotonin Reuptake Inhibitors (SSRIs) often serve as first-line medications for depression and anxiety in Parkinson’s patients. These medications increase serotonin availability in the brain, helping to regulate mood. Common examples include sertraline, escitalopram, and fluoxetine.
For patients who don’t respond adequately to SSRIs, Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) like venlafaxine or duloxetine may provide better results by targeting multiple neurotransmitter systems. In some cases, physicians might prescribe bupropion, which affects dopamine and norepinephrine with minimal sexual side effects.
Anti-anxiety medications such as benzodiazepines may be prescribed for short-term management of severe anxiety, though their use requires careful monitoring due to potential for dependence and cognitive side effects. For longer-term anxiety management, buspirone represents a non-addictive alternative.
Non-Pharmacological Approaches
Exercise delivers powerful mood-enhancing benefits through multiple mechanisms. Physical activity stimulates the release of endorphins, increases neurotransmitter activity, reduces inflammation, and improves sleep quality—all contributing to better mood. Even moderate exercise adapted to individual capabilities can provide significant psychological benefits.
Support groups offer validation, practical advice, and community for those navigating the complex emotional landscape of Parkinson’s disease. Sharing experiences with others who truly understand can significantly reduce feelings of isolation and helplessness.
Mindfulness meditation and relaxation techniques help patients develop greater awareness of thought patterns while reducing physiological stress responses. These practices complement cognitive behavioral therapy for anxiety by teaching individuals to observe thoughts without becoming entangled in them.
Addressing Apathy and Fatigue
Apathy—characterized by diminished motivation, interest, and emotional responsiveness—affects up to 40% of Parkinson’s patients. Often confused with depression, apathy represents a distinct symptom requiring specific interventions.
While depression typically involves sadness and psychological pain, apathy manifests as emotional flatness and reduced initiative. Patients may recognize their lack of motivation but feel neither distressed nor concerned about it. This distinction helps guide appropriate treatment approaches.
Structured routines, scheduled activities, and external motivational supports can help manage apathy. Cognitive behavioral therapy techniques can be adapted to address apathy by establishing behavioral activation strategies and reinforcing the connection between activities and positive outcomes.
Fatigue in Parkinson’s disease stems from multiple factors, including the disease process itself, medication side effects, poor sleep, depression, and the increased energy expenditure required for daily activities. Management approaches include energy conservation techniques, strategic activity scheduling, and addressing underlying contributors like sleep disorders or depression.
Conclusion
Depression and anxiety in Parkinson’s disease represent complex challenges requiring comprehensive management approaches. By understanding the biological basis of these mood disorders and distinguishing them from normal emotional responses to chronic illness, patients and healthcare providers can implement effective treatment strategies.
Cognitive behavioral therapy for burnout offers valuable tools for managing the psychological aspects of Parkinson’s disease. When combined with appropriate medication and lifestyle modifications, CBT can significantly improve quality of life and functional capacity despite the challenges of living with a progressive neurological condition.
BrainTalking encourages individuals with Parkinson’s disease to discuss mood symptoms with healthcare providers and explore the full range of treatment options available. With proper support and intervention, many patients experience substantial improvement in mood and overall well-being, enhancing their ability to manage the broader challenges of Parkinson’s disease.
FAQs About Cognitive Behavioral Therapy for Parkinson’s-Related Depression

How is cognitive behavioral therapy different from regular talk therapy for Parkinson’s patients?
Unlike traditional talk therapy that might focus on exploring past experiences and relationships, cognitive behavioral therapy is present-focused and highly structured. CBT specifically targets the connection between thoughts, feelings, and behaviors that maintain depression and anxiety. For Parkinson’s patients, this means identifying how thoughts about their condition affect mood and developing practical strategies to challenge unhelpful thinking patterns. CBT typically involves homework assignments, specific skill-building exercises, and measurable goals, making it particularly effective for addressing the practical challenges of living with Parkinson’s disease.
Can cognitive behavioral therapy help with medication adherence in Parkinson’s disease?
Yes, cognitive behavioral therapy can significantly improve medication adherence by addressing the psychological barriers that often interfere with consistent medication use. CBT helps patients identify and challenge negative beliefs about medications, develop practical routines and reminders, and create problem-solving strategies for common adherence challenges. Additionally, by treating depression and anxiety that often accompany Parkinson’s disease, CBT can improve overall functioning and motivation, making patients more likely to follow through with their prescribed medication regimens.




