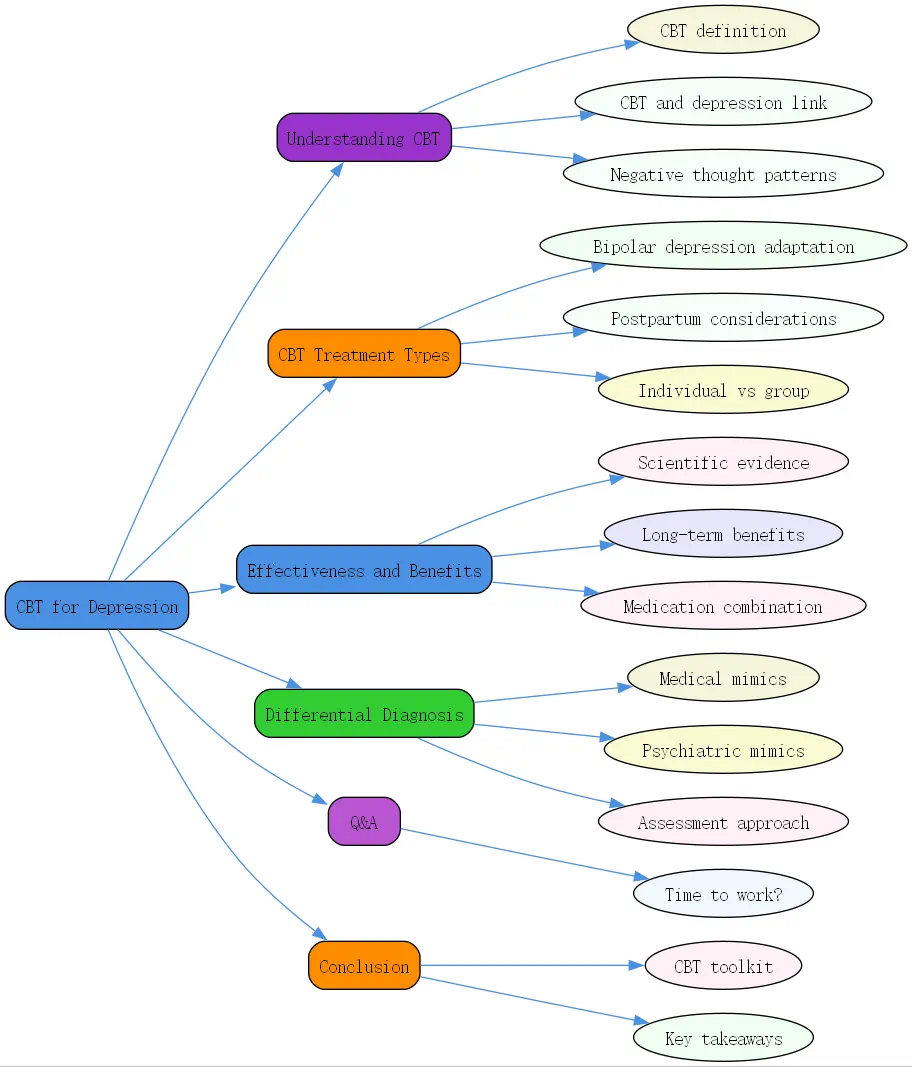
Depression can feel overwhelming, like a shadow that dims even the brightest moments. But there’s a way through it. At BrainTalking, we’re passionate about sharing evidence-based solutions to lighten that load. One of the most powerful tools is Cognitive Behavioral Therapy (CBT). This guide dives into how CBT for depression works, its tailored applications, and why understanding what’s really depression matters. Let’s explore this together.
Understanding CBT and Depression
What is CBT (Cognitive Behavioral Therapy)?
CBT is a structured, goal-oriented form of psychotherapy. It zeroes in on how thoughts, emotions, and behaviors intertwine. The idea? Negative thoughts can trap you in a cycle of distress. By challenging these patterns, CBT helps you shift your mindset and actions. It’s practical, often short-term (think 12-20 sessions), and backed by decades of research. Unlike some therapies, it’s less about digging into your past and more about equipping you for the present.
Why does this matter for depression? Because it’s not just “talking it out.” CBT gives you tools—real, actionable strategies—to tackle the mental habits feeding your low mood. It’s like a mental workout, building resilience step by step.
The Link Between CBT and Depression
Depression often comes with a soundtrack of harsh self-talk: “I’m a failure,” or “Things will never improve.” These thoughts aren’t just passing clouds—they deepen the gloom, making it hard to move forward. CBT steps in by targeting this cycle. It’s built on the premise that distorted thinking fuels depression, and by rewiring those thoughts, you can lift your spirits.
Research shows CBT is a game-changer for many. It’s not about pretending everything’s fine—it’s about seeing reality more clearly. For someone with depression, that shift can feel like turning on a light in a dark room.
How CBT Addresses Negative Thought Patterns
So, how does CBT actually work its magic? It’s all about techniques. Take cognitive restructuring: you spot a thought like “I’ll never get better,” then test it. Is it true? What’s the evidence? Often, you’ll find it’s exaggerated, and you replace it with something balanced, like “I’m struggling now, but I can improve with effort.”
Then there’s behavioral activation. Depression loves isolation—CBT fights that by nudging you toward activities you once enjoyed, or new ones that spark a bit of joy. Over time, these small wins build momentum, proving your thoughts don’t have to run the show.
CBT Treatment for Depression: Types and Applications
CBT for Bipolar Depression: Adapting Therapy
Bipolar depression isn’t your typical low mood—it’s part of a bigger picture with manic highs. CBT for bipolar depression adapts to this complexity. Therapists might focus on mood tracking to spot patterns, or teach skills to manage both dips and spikes. It’s not a standalone fix—medication often plays a role—but CBT adds a layer of control.
What’s unique here? It’s about balance. During depressive phases, it tackles hopelessness; during mania, it curbs impulsivity. Studies suggest this combo approach reduces relapse rates, making it a lifeline for those navigating bipolar’s ups and downs.
CBT for Postpartum Depression: Specific Considerations
New moms facing postpartum depression deal with a whirlwind—hormones, sleep loss, and big life changes. CBT for postpartum depression tailors itself to these challenges. It might address guilt (“I’m not a good mom”) or exhaustion-driven negativity. Sessions could be one-on-one or in groups, offering both personalized help and a sense of community.
The beauty of CBT here? It’s flexible. A therapist might weave in practical coping tips, like managing stress between feedings. For many moms, it’s a path back to feeling like themselves again.
Individual vs. Group CBT Therapy for Depression
Should you go solo or join a group? Individual CBT offers a deep dive—your therapist tailors every session to you. It’s ideal if your depression feels intensely personal or complex. Group CBT, though, brings connection. Hearing others’ struggles can normalize yours, and you learn from their wins.

Both work well. Research from 2025 shows similar outcomes, but groups can be more cost-effective and less isolating. It’s about what fits—some crave privacy, others thrive with peers.
Effectiveness and Benefits of CBT for Depression
Scientific Evidence Supporting CBT for Depression
CBT isn’t just feel-good talk—it’s got solid proof behind it. A 2025 review in the Journal of Clinical Psychology found CBT cuts depressive symptoms by up to 50% in many cases. It’s a first-line treatment per the American Psychological Association, rivaling meds in effectiveness. Why? It targets the root: those pesky thought patterns.
Real-world results back this up. Patients often see gains in weeks, with benefits sticking around long after therapy ends. For anyone doubting, the data’s clear: CBT for depression delivers.
Long-Term Benefits of CBT and Depression Management
Here’s where CBT shines: it’s not a quick fix that fades. It teaches skills—like spotting negative spirals or staying active—that last a lifetime. Think of it as mental armor. Studies show lower relapse rates compared to medication alone, because you’re not just masking symptoms; you’re rewriting the script.
At BrainTalking, we’ve seen this firsthand. Clients say it’s like learning to fish—you don’t just get fed, you master the rod. That’s empowerment, and it’s why CBT stands out.
Combining CBT with Medication for Optimal Results
Sometimes, depression hits hard, and meds can lift the fog enough to let CBT work. Antidepressants tackle chemical imbalances; CBT builds coping tools. Together? A 2025 study found this duo outperforms either alone for severe cases, speeding recovery and cutting relapse risk.
It’s not one-size-fits-all. Mild depression might not need pills, but for tougher battles, this tag-team approach can be a game-changer. Talk to your provider—it’s about finding your balance.
Is It Depression? Differential Diagnosis
Medical Conditions Mimicking Depression
Not every low mood is depression. Medical culprits can masquerade as it—like hyperthyroidism, with its fatigue and irritability, or arrhythmias causing jittery exhaustion. Even caffeine overload or meds like Adderall can mimic depressive slumps. Alcohol withdrawal’s another sneaky one, spiking anxiety that feels like despair.
Ruling these out takes detective work: a solid history, maybe some labs. If your “depression” comes with weight loss or a racing heart, it’s worth a deeper look. Getting it right means better treatment.
Psychiatric Conditions Similar to Depression
Depression doesn’t always travel alone. Generalized anxiety disorder often tags along, with worry that feels depressive. Panic disorder’s intense fear bursts can overlap too. Then there’s bipolar disorder—its lows mimic depression, but mania sets it apart. Confusing them? Risky, since treatments differ.
Check out our piece on anxiety and depression for more on this overlap. A skilled therapist or doctor can untangle the threads—crucial for targeting the real issue.
Assessing Depression: A Thorough Approach
Diagnosing depression isn’t a checklist—it’s an art. Start with a deep patient history: when did it start? What’s it feel like? The “Old Cart” method—Onset, Location, Duration, Character, Aggravating factors, Relieving factors, Timing—digs into details. Add in meds, supplements, life stressors.
Testing? Maybe, if red flags (like thyroid issues) pop up. Otherwise, it’s clinical judgment. A rushed call risks missing the mark—thoroughness ensures CBT or other treatments hit the bullseye.
Q&A Section
Q: How long does CBT take to work for depression?
A: It varies. CBT treatment for depression typically spans 12-20 sessions—about 3-5 months if weekly. Some feel lighter in a few weeks; others need more time, especially with severe symptoms. Consistency’s key: doing the homework, like tracking thoughts, speeds progress. Studies say most see solid gains by session 12, but your pace depends on you and your therapist’s plan.
Conclusion
CBT for depression isn’t just therapy—it’s a toolkit for reclaiming your mind. From tackling bipolar depression to easing postpartum struggles, it adapts to your fight. Backed by science, it offers lasting skills, often boosted by meds when needed. At BrainTalking, we’re here to guide you through it. Not sure it’s depression? Dig deeper with a pro. Help’s out there—brighter days are too.

- CBT rewires negative thoughts, easing depression effectively.
- Tailored for bipolar, postpartum, or classic depression, it’s versatile.
- Evidence shows it works—alone or with meds—for lasting relief.
- Rule out medical or psychiatric mimics for the right diagnosis.
- Start with a thorough assessment; CBT’s power lies in precision.
Explore more mental health insights at BrainTalking!




