Anxiety in Parkinson’s Disease: Identification and Management
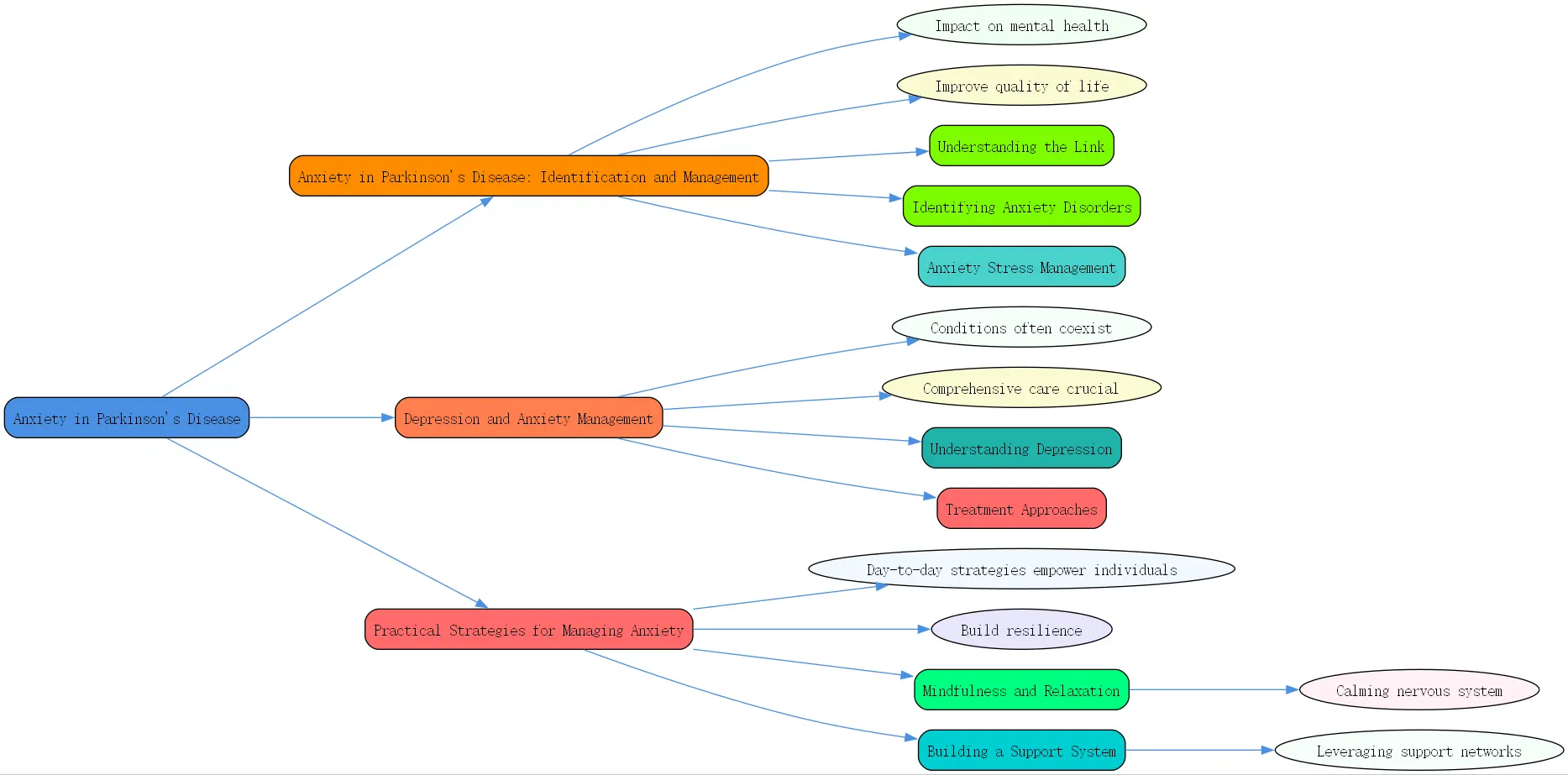
Living with Parkinson’s disease (PD) presents unique physical challenges, but the impact on mental health, particularly anxiety, is equally significant and deserves focused attention. Understanding and addressing these emotional aspects is crucial for maintaining overall well-being. Effective anxiety in parkinson’s disease identification and management is not just about treating symptoms; it’s about improving quality of life and empowering individuals to navigate their journey with greater resilience. This guide explores the complexities of anxiety in PD, drawing on expert insights.
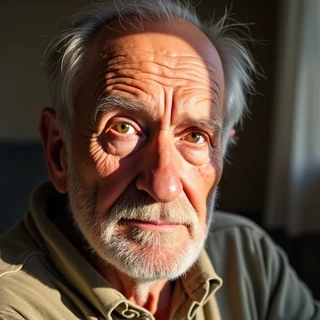
Understanding the Link Between Parkinson’s and Mental Health
The connection between Parkinson’s disease and mental health concerns like anxiety and depression is profound. These aren’t merely reactions to receiving a difficult diagnosis or coping with physical limitations; they are often intrinsically linked to the neurobiological changes occurring within the brain as part of the disease itself. Recognizing this link is the first step toward comprehensive care.
- Prevalence of Anxiety and Depression in Parkinson’s Disease
Statistics reveal a startling reality: at least half of all individuals diagnosed with Parkinson’s will experience significant anxiety or depression at some point during their illness. As expert Dr. Greg Ponton, Associate Professor at Johns Hopkins University School of Medicine, highlights, these conditions are highly prevalent. This underscores the need for proactive screening and open conversations about mental well-being as part of routine Parkinson’s care. Ignoring these symptoms can significantly detract from quality of life.
- The Role of Neurosychiatry in Managing Parkinson’s
The field of neuros psychiatry plays a vital role in understanding and treating the mental health aspects of neurological disorders like Parkinson’s. Specialists in this area, like Dr. Ponton, focus on the intricate intersection of brain health, neurological function, and psychiatric symptoms. They understand that treatments for neurological issues can have psychiatric side effects, and psychiatric medications can impact neurological function, requiring a careful, integrated approach to patient care.
- The Biological Basis of Mental Illness in Parkinson’s Patients
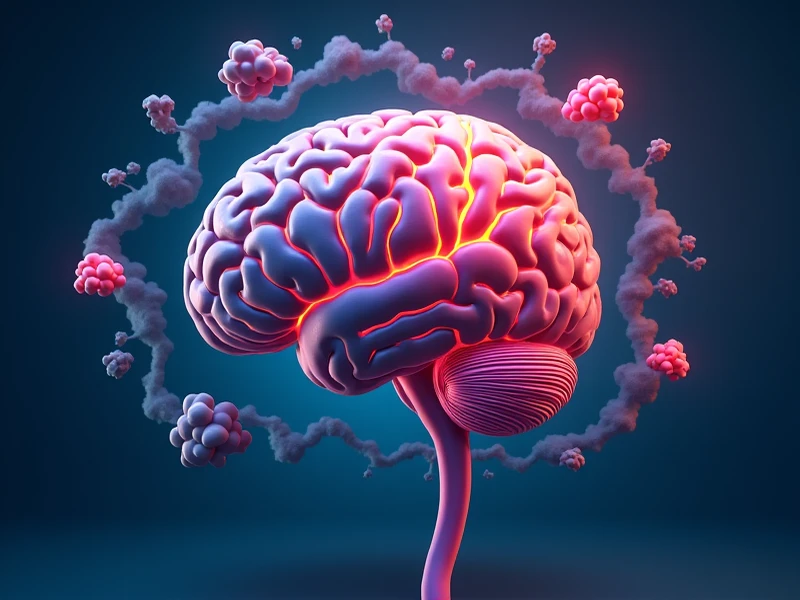 It’s crucial to shift the perspective away from viewing anxiety or depression solely as psychological reactions. Dr. Ponton emphasizes that mental illness, much like PD itself, often has a biological basis rooted in brain chemistry and function. Changes in neurotransmitters like dopamine, serotonin, and norepinephrine, which are affected by Parkinson’s, also play key roles in mood regulation. Acknowledging this biological component helps reduce stigma and underscores the need for medical evaluation and appropriate treatment strategies.
It’s crucial to shift the perspective away from viewing anxiety or depression solely as psychological reactions. Dr. Ponton emphasizes that mental illness, much like PD itself, often has a biological basis rooted in brain chemistry and function. Changes in neurotransmitters like dopamine, serotonin, and norepinephrine, which are affected by Parkinson’s, also play key roles in mood regulation. Acknowledging this biological component helps reduce stigma and underscores the need for medical evaluation and appropriate treatment strategies.
Identifying Anxiety Disorders in Parkinson’s Patients
Distinguishing between the normal stresses of life and a clinical anxiety disorder is vital for effective management, especially within the context of Parkinson’s disease. Anxiety in PD can manifest in various ways, sometimes overlapping with the physical symptoms of the disease itself, making accurate identification essential. Proper `depression and anxiety management` starts with recognizing specific patterns.
- Generalized Anxiety Disorder (GAD) and its Symptoms
Generalized Anxiety Disorder, or GAD, is characterized by persistent, excessive worry about various things, often everyday concerns, that is difficult to control. As Dr. Ponton describes, individuals with GAD might constantly feel tense, have “”butterflies”” in their stomach, or experience physical symptoms like heart palpitations alongside their worries. In Parkinson’s, this worry might latch onto disease progression, medication side effects, social situations, or future uncertainties, becoming pervasive and disruptive.
- Panic Disorder: Recognizing and Managing Panic Attacks
Unlike the constant hum of GAD, panic disorder involves sudden, intense episodes of fear or anxiety that peak within minutes. These panic attacks often come with strong physical symptoms: hyperventilation, racing heart, sweating, trembling, shortness of breath, or feeling a loss of control. Dr. Ponton notes these attacks can sometimes occur “”out of the blue.”” For someone with PD, a panic attack could potentially be triggered by a freezing episode or fear of falling, further complicating the picture. Effective `generalised anxiety disorder and panic disorder in adults management` requires recognizing these distinct episodes.
- Differentiating Normal Anxiety from Anxiety Disorders
Everyone experiences anxiety during times of acute stress – a job interview, a difficult diagnosis, or a challenging event. This is a normal human emotion. However, as Dr. Ponton clarifies, an anxiety disorder is different. It’s characterized by anxiety that is persistent, excessive, significantly interferes with daily functioning (work, relationships, self-care), and causes considerable distress. If anxiety prevents you from engaging in activities you normally would or significantly impacts your quality of life, it’s likely more than just transient stress and warrants professional evaluation.
Anxiety Stress Management Techniques for Parkinson’s
Managing anxiety when living with Parkinson’s requires a proactive and multifaceted approach. It involves not just reacting to anxious feelings but actively cultivating mental wellness and employing specific strategies to cope with both general life stressors and those unique to PD. Integrating effective `anxiety stress management techniques` into daily life is key.
- Active Pursuit of Mental Health and Wellness
 Mental health isn’t merely the absence of illness; Dr. Ponton aligns with the World Health Organization’s view that it’s an optimal state of well-being. Achieving this, especially with the added challenges of PD, requires an “”active pursuit.”” This means consciously making choices and engaging in activities that support emotional and mental resilience. Wellness can be seen as the “”verb”” – the actions taken to achieve that optimal state of health.
Mental health isn’t merely the absence of illness; Dr. Ponton aligns with the World Health Organization’s view that it’s an optimal state of well-being. Achieving this, especially with the added challenges of PD, requires an “”active pursuit.”” This means consciously making choices and engaging in activities that support emotional and mental resilience. Wellness can be seen as the “”verb”” – the actions taken to achieve that optimal state of health.
- The Importance of Physical Health in Managing Anxiety
The mind-body connection is undeniable. Dr. Ponton stresses that taking care of your physical health directly benefits your mental state, and vice versa. Regular physical activity appropriate for your condition, a balanced diet, and adequate sleep are foundational pillars for managing anxiety. Exercise, in particular, releases endorphins and can reduce muscle tension, providing a natural mood boost and anxiety relief. Prioritizing physical wellness is a powerful tool in your anxiety management toolkit.
- Coping Strategies for Social Dilemmas and Disease-Related Stress
People with Parkinson’s are managing the “”big wagon”” of their condition alongside everyday life pressures. Developing robust coping strategies is essential. This includes problem-solving skills for practical challenges, acceptance techniques for things outside one’s control, effective communication strategies for expressing needs, and setting realistic expectations. Learning to navigate social situations that may feel stressful due to symptoms (like tremors or speech changes) is also important.
Depression and Anxiety Management in Parkinson’s Disease
While distinct, depression and anxiety often coexist in individuals with Parkinson’s disease. Understanding the specific symptoms of depression, alongside anxiety, is crucial for comprehensive care. Effective `depression and anxiety management` addresses both conditions, recognizing their potential interplay and combined impact on well-being.
Understanding Depression in Parkinson’s
Depression in Parkinson’s is more than just feeling sad; it’s a clinical syndrome with specific symptoms that significantly impair function. Recognizing these signs is the first step towards getting help. The symptoms can sometimes overlap with PD motor symptoms, making diagnosis challenging but essential.
- Symptoms of Major Depressive Disorder
Dr. Ponton outlines the common constellation of symptoms seen in major depression. A key feature is often anhedonia – a diminished ability to find pleasure in activities previously enjoyed. Other common signs include persistent sadness or low mood, significant sleep disturbances (usually insomnia), appetite changes (often loss and weight loss), pervasive low energy and lack of initiative, feelings of worthlessness or excessive guilt, difficulty concentrating, and, in severe cases, thoughts of death or suicide.
- Atypical Depression: Recognizing Less Common Symptoms
While less common, some individuals experience what’s termed atypical depression. Instead of insomnia and appetite loss, they might experience hypersomnolence (sleeping excessively, perhaps 15-16 hours a day) and increased appetite or “”comfort eating,”” potentially leading to weight gain. Recognizing these less typical patterns is important for accurate diagnosis and treatment.
- The Impact of Depression on Daily Function
Depression significantly impacts a person’s ability to function optimally. It saps motivation, makes even simple tasks feel overwhelming, strains relationships, and diminishes overall quality of life. When combined with the physical challenges of Parkinson’s, depression can create a heavy burden, potentially worsening motor symptoms and reducing adherence to treatments. Addressing depression is therefore critical for overall PD management.
Treatment Approaches for Depression and Anxiety
Fortunately, both depression and anxiety in Parkinson’s are treatable. A comprehensive approach often combines medication, therapy, and lifestyle adjustments, tailored to the individual’s specific needs and considering the complexities of PD. Collaboration between neurologists, psychiatrists, therapists, and the patient is key.
- Medication Options and Considerations
Various antidepressant and anti-anxiety medications can be effective. However, careful selection is crucial in PD due to potential interactions with Parkinson’s medications or the possibility of worsening certain motor symptoms. Selective Serotonin Reuptake Inhibitors (SSRIs) are often considered first-line options. Close monitoring by a physician experienced in treating mental health conditions in PD patients, possibly a neuros psychiatrist, is essential.
- Therapeutic Interventions: Cognitive Behavioral Therapy (CBT) and Counseling
Talk therapies provide invaluable tools for managing both depression and anxiety. Cognitive Behavioral Therapy (CBT) is particularly effective; it helps individuals identify and challenge negative thought patterns and develop healthier coping behaviors. General counseling provides a supportive space to process emotions and develop strategies. Therapy equips individuals with long-term `anxiety stress management techniques`.
- Lifestyle Adjustments: Diet, Exercise, and Sleep Hygiene
Lifestyle factors form the bedrock of mental health management. Consistent, appropriate exercise boosts mood and reduces anxiety. A balanced diet supports brain health. Good sleep hygiene – maintaining a regular sleep schedule, creating a restful environment, and avoiding stimulants before bed – is critical, as sleep disturbances are common in both PD and mood disorders. These adjustments support overall well-being and enhance the effectiveness of other treatments.
Practical Strategies for Managing Anxiety in Parkinson’s
Beyond formal treatments, incorporating practical, day-to-day strategies can significantly empower individuals to manage anxiety associated with Parkinson’s disease. These techniques focus on calming the nervous system, building resilience, and leveraging support networks, forming a crucial part of holistic anxiety in parkinson’s disease identification and management.
Mindfulness and Relaxation Techniques
Actively engaging in relaxation practices can counteract the physiological effects of anxiety and promote a sense of calm. These techniques are accessible and can be adapted for varying levels of mobility, making them valuable tools for individuals with PD. Consistent practice yields the best results.
- Deep Breathing Exercises for Stress Reduction
Simple diaphragmatic breathing (deep belly breathing) can quickly calm the nervous system. Inhaling slowly through the nose, allowing the belly to expand, and exhaling slowly through the mouth signals relaxation to the brain. Practicing this regularly, and especially during moments of rising anxiety, can provide immediate relief and is a fundamental `anxiety stress management technique`.
- Meditation and Mindfulness Practices
Mindfulness involves paying attention to the present moment without judgment. This can involve focusing on the breath, bodily sensations, or external sounds. Meditation apps (some free, others requiring subscription, like the ‘Elevate’ app mentioned by Dr. Ponton’s interviewer, though many others exist) can guide practice. Mindfulness helps detach from anxious thoughts about the past or future, grounding you in the now.
- Progressive Muscle Relaxation
This technique involves systematically tensing and then releasing different muscle groups throughout the body. By consciously tensing muscles (e.g., clenching fists) for a few seconds and then releasing the tension, you become more aware of physical tension and learn to induce relaxation. This can be particularly helpful for the muscle rigidity sometimes associated with PD.
Building a Support System
Navigating Parkinson’s and anxiety is not a journey meant to be taken alone. A strong support system provides emotional resilience, practical assistance, and shared understanding, which are invaluable components of effective management. Isolation can exacerbate anxiety, making connection vital.
- The Role of Care Partners in Anxiety Management
Care partners – spouses, family members, or close friends – often play a crucial role. They may be the first to notice changes in mood or behavior indicative of anxiety or depression. They provide emotional support, can assist with implementing management strategies (like encouraging exercise or relaxation practice), and help facilitate communication with healthcare providers. Open communication within this partnership is key.
- Support Groups for Parkinson’s Patients and Families
Connecting with others who understand the unique challenges of living with Parkinson’s can be incredibly validating and empowering. Support groups (in-person or online) offer a space to share experiences, exchange coping strategies, learn from peers, and reduce feelings of isolation. Organizations like the Davis Phinney Foundation (mentioned in the reference text) often provide resources for finding local groups.
- Seeking Professional Help: When to Consult a Specialist
While self-help strategies and support groups are beneficial, professional help is often necessary. If anxiety or depression symptoms are persistent, severe, or significantly impacting daily life, consulting a healthcare professional is crucial. This might start with a primary care physician or neurologist, who can then refer to a psychiatrist, psychologist, therapist, or ideally, a neuros psychiatrist familiar with Parkinson’s disease for specialized care.
Key Takeaways for Managing Anxiety in Parkinson’s:
- Acknowledge Prevalence: Anxiety and depression affect at least 50% of people with PD; you are not alone.
- Recognize the Biology: Mental health issues in PD often have a biological basis linked to brain changes, not just situational stress.
- Identify Symptoms: Learn to distinguish between GAD (persistent worry) and Panic Disorder (acute attacks), and differentiate them from normal stress.
- Pursue Wellness Actively: Mental health requires conscious effort through lifestyle choices and coping strategies.
- Prioritize Physical Health: Exercise, diet, and sleep are foundational for managing anxiety and depression.
- Utilize Practical Techniques: Incorporate deep breathing, mindfulness, and relaxation into your routine.
- Build Your Support: Lean on care partners, connect with support groups, and don’t hesitate to seek professional help.
- Seek Integrated Care: Effective management often involves collaboration between neurologists, mental health professionals, and potentially neuros psychiatrists.
Q: How can I tell if my feelings of worry are just stress or an actual anxiety disorder related to my Parkinson’s?
A: This is a common and important question. Differentiating normal stress from a clinical anxiety disorder involves looking at intensity, duration, triggers, and impact on functioning. Normal anxiety is usually tied to a specific, identifiable stressor (e.g., an upcoming doctor’s appointment) and tends to lessen once the situation resolves. While unpleasant, it generally doesn’t stop you from carrying out your daily responsibilities.