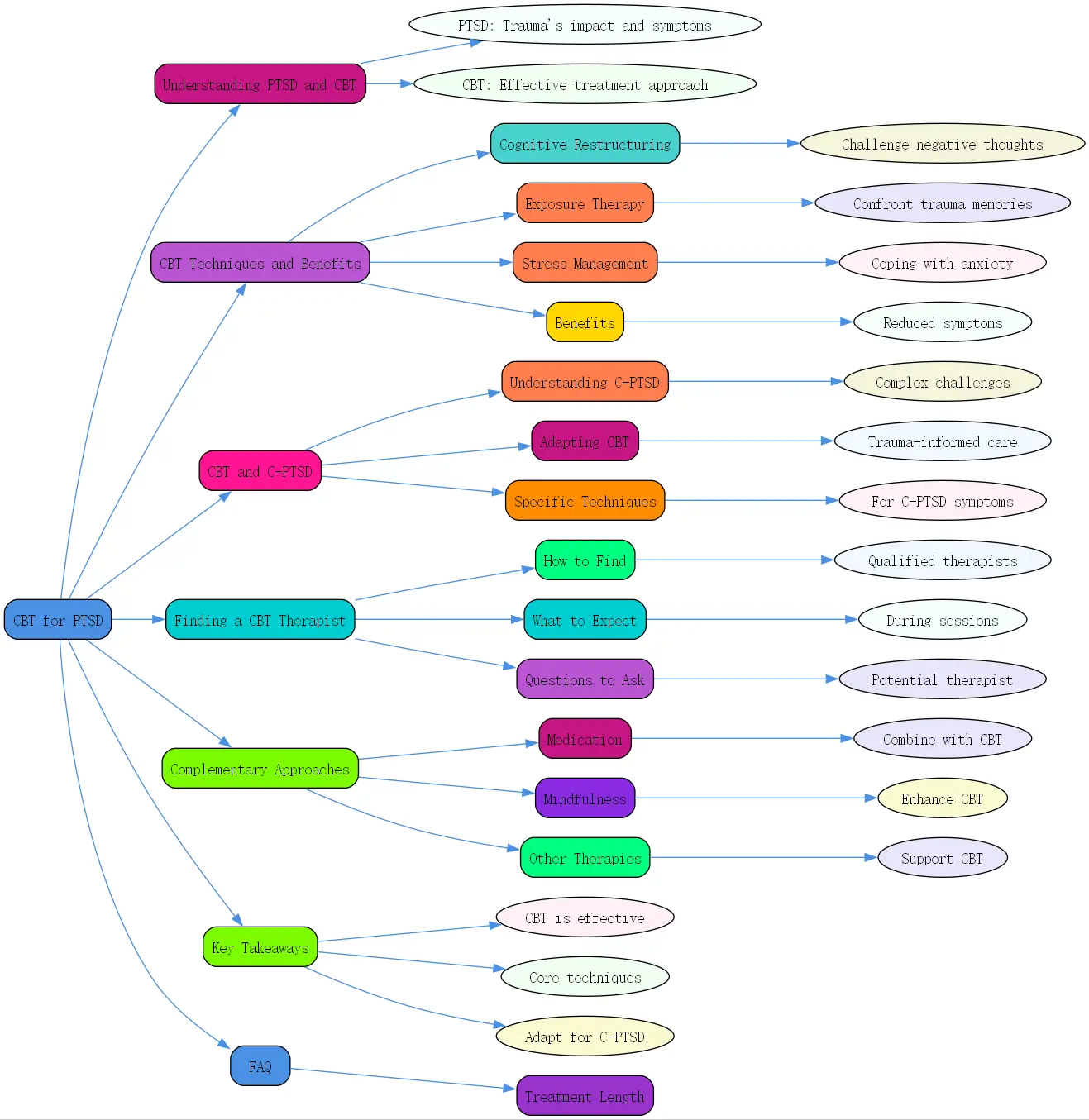
Understanding PTSD and the Role of CBT
Post-Traumatic Stress Disorder (PTSD) is a debilitating condition that can develop after experiencing or witnessing a traumatic event. The impact of trauma extends far beyond momentary fear, often reshaping how individuals perceive themselves and the world around them. Those suffering from PTSD frequently experience intrusive memories, nightmares, heightened anxiety, and avoidance behaviors that significantly interfere with daily functioning.
Trauma profoundly affects both the brain and body. When experiencing trauma, the brain’s alarm system—particularly the amygdala—becomes hyperactive, while the prefrontal cortex, responsible for rational thinking, often shows reduced activity. This neurobiological impact explains why trauma survivors might remain in a perpetual state of “”fight or flight,”” even when no immediate danger exists. Physical manifestations can include sleep disturbances, heightened startle responses, and chronic tension.

Cognitive Behavioral Therapy (CBT) has emerged as one of the most effective treatments for PTSD. This structured, evidence-based approach focuses on identifying and modifying unhelpful thoughts and behaviors that maintain trauma symptoms. Unlike some therapy approaches that primarily explore past experiences, CBT equips individuals with practical skills to manage symptoms and reclaim their lives. Research consistently demonstrates that CBT for PTSD yields significant improvements, often within 12-16 sessions.
CBT Treatment for PTSD: Techniques and Benefits
Cognitive Restructuring: Identifying and Challenging Negative Thoughts
Cognitive restructuring forms a cornerstone of CBT for PTSD treatment. This technique helps individuals identify distorted thought patterns that developed following trauma. Common distortions include catastrophizing (“”Something terrible will happen again””), self-blame (“”It was my fault””), and overgeneralization (“”Nowhere is safe””). Through guided exploration, therapists help clients examine evidence for and against these beliefs.
The process involves keeping thought records to track negative automatic thoughts and their emotional impact. Clients learn to recognize how these thoughts fuel anxiety and avoidance behaviors. With practice, individuals develop the ability to generate more balanced alternatives that acknowledge both their trauma and their capacity for healing. This cognitive shift doesn’t minimize the trauma but creates mental space for recovery and growth.
Exposure Therapy: Gradually Confronting Trauma-Related Memories and Situations
Exposure therapy represents another powerful component of CBT for complex PTSD. This technique involves systematically confronting trauma-related memories, thoughts, and situations that trigger distress. The fundamental principle is that avoidance, while providing temporary relief, ultimately reinforces fear and prevents recovery. By facing these triggers in a controlled, supportive environment, their emotional power gradually diminishes.

Therapists typically begin with imaginal exposure, where clients verbally recount their traumatic experience in present tense, often recording the narrative for repeated listening. In vivo exposure involves facing real-world situations that have been avoided due to trauma associations. Throughout this process, clients learn that anxiety naturally decreases with continued exposure—a phenomenon called habituation. This approach has proven particularly effective for reducing flashbacks and nightmares associated with PTSD.
Stress Management Techniques: Coping Skills for Anxiety and Arousal
CBT treatment for PTSD incorporates various stress management techniques to help individuals regulate their physiological responses to triggers. These include diaphragmatic breathing, progressive muscle relaxation, and grounding exercises that redirect attention to the present moment. These skills provide immediate relief during moments of distress and serve as alternatives to unhealthy coping mechanisms.
Mindfulness practices train individuals to observe thoughts and sensations without judgment, creating distance from overwhelming emotions. Many clients benefit from worksheets for anxiety management that guide them through these exercises. Regular practice of these techniques can actually reshape neural pathways, making the stress response system less reactive over time.
Benefits of CBT: Reduced Symptoms, Improved Coping, Enhanced Quality of Life
The benefits of CBT and PTSD treatment extend far beyond symptom reduction. Research consistently shows that successful CBT interventions lead to significant improvements in overall functioning and quality of life. Many clients report decreased intrusive thoughts, reduced hypervigilance, and fewer avoidance behaviors. Sleep quality often improves dramatically, enhancing overall well-being.
Beyond symptom relief, CBT equips individuals with lifelong skills for managing stress and difficult emotions. This increased sense of self-efficacy—the belief in one’s ability to handle challenges—often translates to improvements in relationships, work performance, and engagement in meaningful activities. Many clients describe a profound shift from feeling controlled by their trauma to feeling empowered in their recovery journey.
CBT and PTSD: Addressing Complex Trauma (C-PTSD)
Understanding Complex PTSD and Its Unique Challenges
Complex PTSD (C-PTSD) develops in response to prolonged, repeated trauma, often occurring in contexts where escape seems impossible. While sharing many symptoms with PTSD, C-PTSD additionally involves difficulties with emotional regulation, negative self-perception, and relationship challenges. Those suffering often experience a profound sense of emptiness, shame, and disconnection from others.
The developmental impact of complex trauma, especially when occurring during childhood, can disrupt fundamental aspects of self-formation. Many survivors struggle with basic trust, boundary-setting, and identifying their own needs and emotions. This complex presentation requires specialized treatment approaches that go beyond standard trauma protocols, addressing both symptom management and these deeper relational and identity-related wounds.
Adapting CBT for C-PTSD: Incorporating Trauma-Informed Care
CBT for complex PTSD requires thoughtful adaptation to address the unique challenges presented by prolonged or repeated trauma. Effective therapy typically extends beyond standard protocols, incorporating principles of trauma-informed care. These include establishing exceptional safety within the therapeutic relationship, moving at a pace that respects the client’s window of tolerance, and acknowledging the valid adaptations that helped the client survive overwhelming circumstances.
At BrainTalking, trauma specialists recognize that complex trauma treatment often requires a longer duration and greater emphasis on building a secure therapeutic alliance before engaging in exposure work. Phase-based approaches typically begin with stabilization and skill-building, ensuring clients have adequate resources before processing traumatic material. This modified framework honors the unique healing journey of each individual while maintaining the evidence-based structure that makes CBT effective.
Specific CBT Techniques for C-PTSD Symptoms
When applying CBT for C-PTSD treatment, therapists employ specialized techniques that address the distinct symptom profile. For emotional dysregulation, dialectical behavior therapy skills (a CBT variant) teach clients to identify emotions, tolerate distress, and implement effective self-soothing strategies. Schema-focused work helps individuals recognize and modify core negative beliefs about themselves that formed during traumatic experiences.
For relationship difficulties, interpersonal effectiveness training provides concrete skills for setting boundaries, communicating needs, and building healthy connections. Additionally, techniques like “”parts work”” acknowledge the different aspects of self that developed to manage trauma, fostering internal cohesion and self-compassion. These adaptations make CBT particularly effective for addressing the multifaceted nature of complex trauma recovery.
Finding a CBT Therapist for PTSD Treatment
How to Find Qualified CBT Therapists
Finding the right therapist for CBT for PTSD requires careful consideration. Start by seeking professionals with specific training in trauma-focused CBT approaches. Look for certifications in evidence-based protocols like Cognitive Processing Therapy (CPT) or Prolonged Exposure (PE). Professional directories from organizations like the Association for Behavioral and Cognitive Therapies or the International Society for Traumatic Stress Studies can guide your search.
Consider asking potential therapists about their experience treating clients with similar trauma backgrounds. Many practitioners offer free phone consultations that provide an opportunity to assess their approach and expertise. Insurance panels, community mental health centers, and university training clinics may also have qualified providers. For veterans, the VA healthcare system offers specialized trauma services incorporating CBT approaches.
What to Expect During CBT Sessions
CBT for PTSD typically follows a structured format while allowing flexibility to address individual needs. Initial sessions focus on assessment, education about PTSD, and collaborative goal-setting. Your therapist will work with you to develop a treatment plan that balances challenging work with respect for your readiness and comfort level.
Regular sessions often begin with a brief check-in, followed by reviewing homework assignments that reinforced skills practiced during previous meetings. The main portion typically involves learning and applying specific CBT techniques, such as cognitive restructuring or exposure exercises. Sessions conclude with summarizing key takeaways and assigning relevant homework. Throughout treatment, your therapist will regularly assess your progress using standardized measures and adjust the approach as needed.
Questions to Ask a Potential Therapist
When interviewing potential therapists for CBT treatment for PTSD, consider asking these essential questions: “”What specific training do you have in trauma-focused CBT approaches?”” “”How do you typically structure treatment for PTSD?”” “”What is your approach to exposure work?”” These questions help assess the therapist’s expertise and treatment philosophy.
Additionally, practical questions like “”How do you handle situations when clients feel overwhelmed during sessions?”” and “”What is your policy on between-session contact?”” provide insight into how the therapist manages distress and supports clients throughout the treatment process. Finally, asking about expected treatment duration and how progress will be measured helps set realistic expectations for the recovery journey.
CBT for PTSD: Complementary Approaches
Combining CBT with Medication for PTSD
For many individuals, combining CBT with appropriate medication provides optimal relief from PTSD symptoms. Selective serotonin reuptake inhibitors (SSRIs), particularly sertraline and paroxetine, have FDA approval for PTSD treatment. These medications can reduce core symptoms like intrusive thoughts, hyperarousal, and avoidance behaviors, creating a foundation for more effective therapeutic work.
The decision to include medication should involve careful consultation with both your therapist and a psychiatrist or primary care physician. Some individuals find that medication provides sufficient symptom relief to engage more fully in CBT work. Others may begin with combined treatment and gradually taper medication as they develop stronger coping skills through therapy. This integrated approach addresses both the neurobiological and psychological dimensions of trauma recovery.
Mindfulness and CBT for PTSD
Mindfulness practices enhance traditional CBT for PTSD by developing present-moment awareness without judgment. These techniques help individuals observe thoughts and sensations without becoming overwhelmed by them, creating space between triggers and reactions. Regular mindfulness practice can reduce rumination about past traumas and worry about future threats, addressing core aspects of PTSD.
Specific mindfulness-based interventions like body scans, breathing exercises, and sensory grounding techniques support trauma recovery by safely reconnecting individuals with their physical experience. These approaches complement cognitive work by enhancing emotional regulation and reducing avoidance. Many clients find that integrating these practices into daily routines provides ongoing support between therapy sessions and sustainable skills for long-term well-being.
Other Therapies That Complement CBT
While CBT provides an excellent foundation for PTSD treatment, several complementary approaches can enhance recovery. Eye Movement Desensitization and Reprocessing (EMDR) uses bilateral stimulation to help process traumatic memories and has strong empirical support. Group therapy offers valuable peer support and normalization of experiences, particularly beneficial for combat veterans or sexual assault survivors.
Somatic (body-centered) therapies address the physical manifestations of trauma that may persist even after cognitive work. Creative arts therapies like art, music, or dance provide alternative expression channels when words feel insufficient. At BrainTalking, therapists often integrate these approaches with CBT principles, creating customized treatment plans that address the full spectrum of trauma’s impact on mind, body, and spirit.
Key Takeaways on CBT for PTSD
- CBT is a highly effective, evidence-based treatment for PTSD that addresses both thoughts and behaviors maintaining symptoms
- Core techniques include cognitive restructuring, exposure therapy, and stress management skills
- Complex PTSD requires specialized adaptations of standard CBT approaches
- Finding a qualified therapist with specific trauma training is essential for effective treatment
- Complementary approaches like medication, mindfulness, and group therapy can enhance CBT outcomes
- Recovery is possible—many people experience significant improvement with appropriate treatment
Frequently Asked Questions
How long does CBT treatment for PTSD typically take?
Standard CBT for PTSD typically ranges from 12-16 weekly sessions, though this varies based on individual needs and trauma complexity. For complex PTSD, treatment often extends longer, sometimes 6-12 months or more. Many clients notice some symptom improvement within the first month of treatment, with substantial gains typically emerging around the 2-3 month mark.





